Monday Poster Session
Category: Stomach
P3312 - Racial Disparities in Post Endoscopy Interval Gastric Cancer: Outcomes From a Nationwide Database
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- RK
Rahul Karna, MD
University of Minnesota Medical Center
Minneapolis, MN
Presenting Author(s)
Rahul Karna, MD1, Natalie Wilson, MD2, Anders Westanmo, PharmD, MBA3, Amy Gravely, MA3, Brian Hanson, MD3, Mohammad Bilal, MD4
1University of Minnesota Medical Center, Minneapolis, MN; 2University of Minnesota, Minneapolis, MN; 3Minneapolis VA Health Care System, Minneapolis, MN; 4University of Minnesota and Minneapolis VA Health Care System, Minneapolis, MN
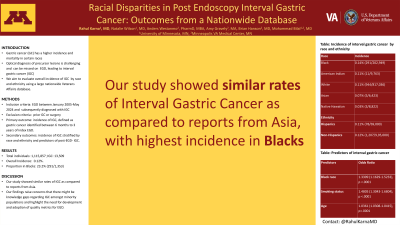
Introduction: Gastric cancer has higher incidence and mortality in population of certain races. Despite high incidence, there is no clear screening guidelines for gastric cancer in the United States. Detection of precursor lesions of gastric cancer can help in risk stratification for future surveillance. However, optical diagnosis of these precursor lesions is challenging and therefore, can be missed on esophagogastroduodenoscopy (EGD) resulting in interval gastric cancer (IGC). We aimed to evaluate overall incidence of IGC after EGD and rates of IGC after EGD by race and ethnicity using a large nationwide Veterans Affairs database.
Methods: Data was obtained from the Veterans Health Administration Corporate Data Warehouse using Structured Query Language (SQL). Individuals who underwent EGD between January 2005-May 2024 and subsequently diagnosed with gastric cancer were included. Patients with history of gastric cancer or gastric surgeries were excluded. Primary outcome was incidence of IGC, defined as gastric cancer identified between 6 months to 3 years of index EGD. Secondary outcomes were incidence of IGC stratified by race and ethnicity and predictors of post-EGD IGC.
Results: A total of 1,115,857 individuals underwent EGD and 13,509 patients were diagnosed with IGC. Gastric cancer diagnosed within 6 months (9,982) and after 36 months (2,174) of index EGD were excluded from analysis. Table 1 shows demographic details of patients with and without IGC. The rate of IGC was in 0.12%. 23.2% (291/1,353) of all IGC were recorded in Blacks. Incidence of IGC were highest in Blacks: 0.14% (291/202,949), followed by American Indian: 0.11% (11/9,763), Whites 0.11% (944/817,036), Asian: 0.07% (5/6,423) and Native Hawaiian: 0.03% (3/8,822). Incidence in Hispanics was: 0.11% (78/69,000) and Non-Hispanics: 0.12% (1,207/9,95,000). On multivariate analysis, independent predictors for IGC included Black race [OR:1.3309 (1.1629-1.5233), p < .0001] along with smoking status [OR: 1.4805 (1.3043-1.6804), p < .0001], age [OR: 1.0361 (1.0308-1.0415), p< .0001] while GERD decreased risk [OR: 0.7565 (0.6675-0.8574), p< .0001].
Discussion: Our study showed similar rates of IGC as compared to reports from Asia. In addition, Blacks were more likely to develop IGC. Our findings raise concerns that there might be knowledge gaps regarding IGC amongst minority populations, and highlight the need for development and adoption of quality metrics for EGD.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Rahul Karna, MD1, Natalie Wilson, MD2, Anders Westanmo, PharmD, MBA3, Amy Gravely, MA3, Brian Hanson, MD3, Mohammad Bilal, MD4. P3312 - Racial Disparities in Post Endoscopy Interval Gastric Cancer: Outcomes From a Nationwide Database, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Minnesota Medical Center, Minneapolis, MN; 2University of Minnesota, Minneapolis, MN; 3Minneapolis VA Health Care System, Minneapolis, MN; 4University of Minnesota and Minneapolis VA Health Care System, Minneapolis, MN
Introduction: Gastric cancer has higher incidence and mortality in population of certain races. Despite high incidence, there is no clear screening guidelines for gastric cancer in the United States. Detection of precursor lesions of gastric cancer can help in risk stratification for future surveillance. However, optical diagnosis of these precursor lesions is challenging and therefore, can be missed on esophagogastroduodenoscopy (EGD) resulting in interval gastric cancer (IGC). We aimed to evaluate overall incidence of IGC after EGD and rates of IGC after EGD by race and ethnicity using a large nationwide Veterans Affairs database.
Methods: Data was obtained from the Veterans Health Administration Corporate Data Warehouse using Structured Query Language (SQL). Individuals who underwent EGD between January 2005-May 2024 and subsequently diagnosed with gastric cancer were included. Patients with history of gastric cancer or gastric surgeries were excluded. Primary outcome was incidence of IGC, defined as gastric cancer identified between 6 months to 3 years of index EGD. Secondary outcomes were incidence of IGC stratified by race and ethnicity and predictors of post-EGD IGC.
Results: A total of 1,115,857 individuals underwent EGD and 13,509 patients were diagnosed with IGC. Gastric cancer diagnosed within 6 months (9,982) and after 36 months (2,174) of index EGD were excluded from analysis. Table 1 shows demographic details of patients with and without IGC. The rate of IGC was in 0.12%. 23.2% (291/1,353) of all IGC were recorded in Blacks. Incidence of IGC were highest in Blacks: 0.14% (291/202,949), followed by American Indian: 0.11% (11/9,763), Whites 0.11% (944/817,036), Asian: 0.07% (5/6,423) and Native Hawaiian: 0.03% (3/8,822). Incidence in Hispanics was: 0.11% (78/69,000) and Non-Hispanics: 0.12% (1,207/9,95,000). On multivariate analysis, independent predictors for IGC included Black race [OR:1.3309 (1.1629-1.5233), p < .0001] along with smoking status [OR: 1.4805 (1.3043-1.6804), p < .0001], age [OR: 1.0361 (1.0308-1.0415), p< .0001] while GERD decreased risk [OR: 0.7565 (0.6675-0.8574), p< .0001].
Discussion: Our study showed similar rates of IGC as compared to reports from Asia. In addition, Blacks were more likely to develop IGC. Our findings raise concerns that there might be knowledge gaps regarding IGC amongst minority populations, and highlight the need for development and adoption of quality metrics for EGD.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Rahul Karna indicated no relevant financial relationships.
Natalie Wilson indicated no relevant financial relationships.
Anders Westanmo indicated no relevant financial relationships.
Amy Gravely indicated no relevant financial relationships.
Brian Hanson: Motus GI – Consultant.
Mohammad Bilal: Boston Scientific – Consultant. Cook endoscopy – Speakers Bureau.
Rahul Karna, MD1, Natalie Wilson, MD2, Anders Westanmo, PharmD, MBA3, Amy Gravely, MA3, Brian Hanson, MD3, Mohammad Bilal, MD4. P3312 - Racial Disparities in Post Endoscopy Interval Gastric Cancer: Outcomes From a Nationwide Database, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
