Monday Poster Session
Category: Stomach
P3315 - Long-Term PPI Therapy Does Not Reduce Serum Calcium Levels: A Meta-Regression Analysis
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E

Has Audio

Tulio L Correa, MD
Beth Israel Deaconess Medical Center, Harvard Medical School
Boston, MA
Presenting Author(s)
Tulio L Correa, MD1, Vanio Antunes, MS2, Matheus V Fernandes, MHS, MD2, Otavio C Martins, MS3, Natalia J Milioli, MD4, Cynthia Florencio De Mesquita, MS5, Stefano Baraldo, MD6, Marco Noriega, MD, MPH7, Javier A Villafuerte-Galvez, MD1
1Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA; 2Federal University of Health Sciences of Porto Alegre, Porto Alegre, Rio Grande do Sul, Brazil; 3Juiz de Fora Federal University, Juiz de Fora, Minas Gerais, Brazil; 4Pontifical Catholic University of Rio Grande do Sul, Porto Alegre, Rio Grande do Sul, Brazil; 5Federal University of Pernambuco, Recife, Pernambuco, Brazil; 6Barretos Cancer Hospital, Barretos, Sao Paulo, Brazil; 7Beth Israel Deaconess Medical Center, Boston, MA
Introduction: Although studies have linked the use of proton pump inhibitors (PPI) to the development of bone fractures and osteoporosis, recent data on the effects of PPIs on calcium absorption have been inconsistent. Therefore, we aimed to perform a meta-analysis to evaluate the associations between PPI use and serum calcium and urinary calcium excretion (UCE) in adults.
Methods: A systematic review of the literature was conducted using the PubMed/Medline, Cochrane Library, and Scopus databases in February 2024. This review included only randomized controlled trials (RCTs) that assessed serum calcium levels or UCE in patients using PPIs compared to non-PPI users. Subgroup statistical analyses with hemodialysis patients, standard- or double-dose, and short- or long-term PPI use were performed. A meta-regression model was conducted with PPI treatment duration as the independent variable. Treatment effects were compared using Standardized Mean Difference (SMD) with 95% confidence intervals (CI).
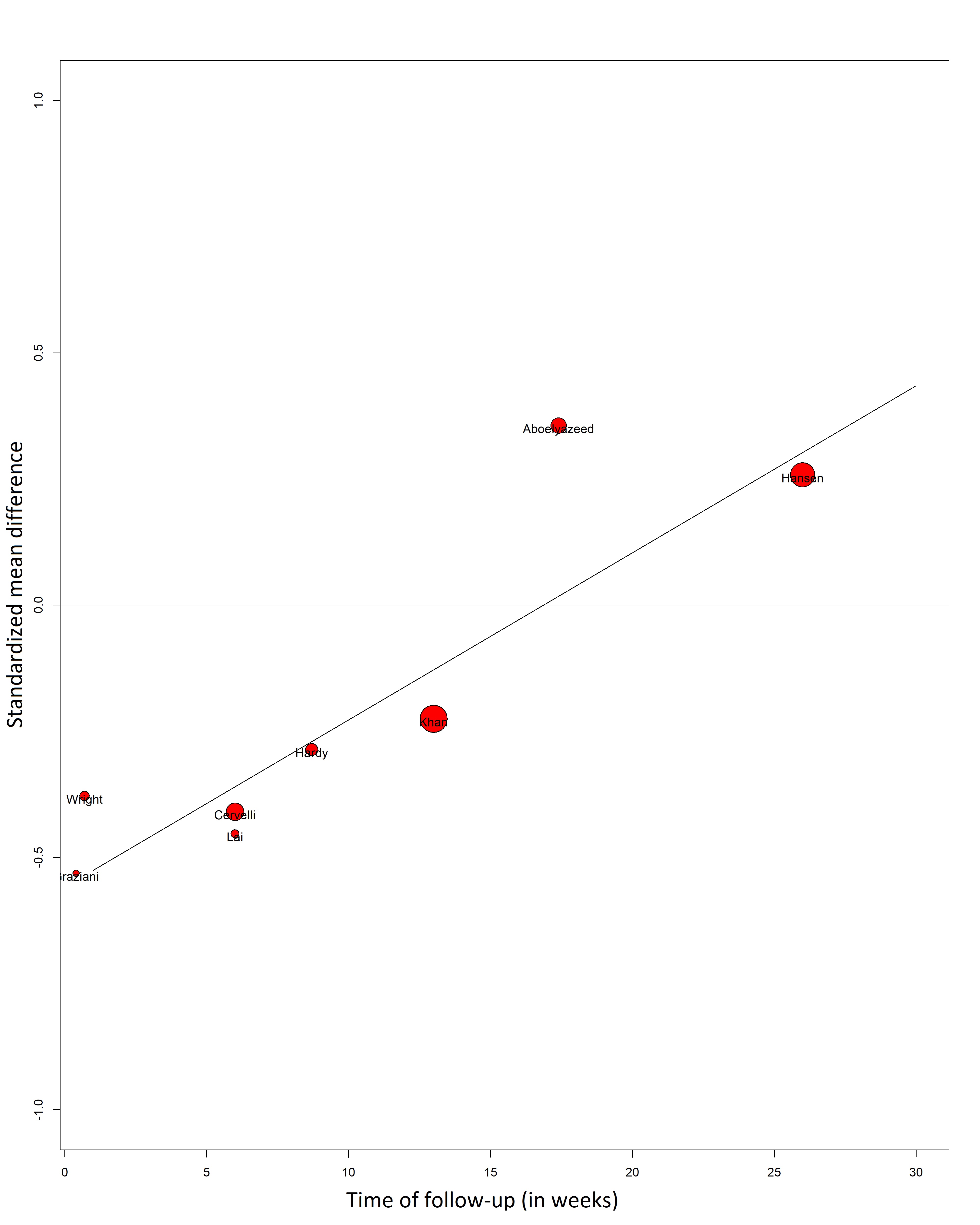
Results: Of the 815 studies initially identified, 8 RCTs (n = 376) evaluated serum calcium and 3 (n = 122) evaluated UCE. PPI users had no statistically significant difference in serum calcium compared to non-PPI users (SMD -0.13; 95% CI -0.38 to 0.12; p = 0.29; I2 = 17%). Subgroup analyses with patients on hemodialysis (SMD -0.19; 95% CI -0.44 to 0.06; p = 0.14; I2 = 4%), non-hemodialysis (SMD -0.09; 95% CI -0.62 to 0.45; p = 0.76; I2 = 38%), standard-dose PPI (SMD -0.17; 95% CI -0.57 to 0.23; p = 0.41; I2 = 27%), double-dose PPI (SMD -0.11; 95% CI -0.47 to 0.24; p = 0.54; I2 = 28%), and long-term PPI users (SMD 0.03; 95% CI -0.29 to 0.34; p = 0.87; I2 = 34%) also showed no significant differences for serum calcium. Non-PPI users had a slightly higher serum calcium than short-term PPI users (SMD -0.43; 95% CI -0.80 to -0.05; p = 0.03; I2 = 0%). Meta-regression analysis showed a tendency towards higher serum calcium in patients with longer PPI treatment duration (R² = 1; p = 0.009) (Figure 1). There was no statistically significant difference regarding UCE (SMD -2.23; 95% CI -5.73 to 1.28; p = 0.21; I2 = 90%).
Discussion: PPI use was not associated with decreased serum calcium levels. Any hypothesized changes in intestinal calcium absorption, if present, are not reflected in serum calcium. Furthermore, UCE, a key compensatory mechanism affected by parathormone remains unchanged. This data raises mechanistic plausibility questions to the hypothesized noxious effect of PPIs on bone density and fracture risk.
Disclosures:
Tulio L Correa, MD1, Vanio Antunes, MS2, Matheus V Fernandes, MHS, MD2, Otavio C Martins, MS3, Natalia J Milioli, MD4, Cynthia Florencio De Mesquita, MS5, Stefano Baraldo, MD6, Marco Noriega, MD, MPH7, Javier A Villafuerte-Galvez, MD1. P3315 - Long-Term PPI Therapy Does Not Reduce Serum Calcium Levels: A Meta-Regression Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA; 2Federal University of Health Sciences of Porto Alegre, Porto Alegre, Rio Grande do Sul, Brazil; 3Juiz de Fora Federal University, Juiz de Fora, Minas Gerais, Brazil; 4Pontifical Catholic University of Rio Grande do Sul, Porto Alegre, Rio Grande do Sul, Brazil; 5Federal University of Pernambuco, Recife, Pernambuco, Brazil; 6Barretos Cancer Hospital, Barretos, Sao Paulo, Brazil; 7Beth Israel Deaconess Medical Center, Boston, MA
Introduction: Although studies have linked the use of proton pump inhibitors (PPI) to the development of bone fractures and osteoporosis, recent data on the effects of PPIs on calcium absorption have been inconsistent. Therefore, we aimed to perform a meta-analysis to evaluate the associations between PPI use and serum calcium and urinary calcium excretion (UCE) in adults.
Methods: A systematic review of the literature was conducted using the PubMed/Medline, Cochrane Library, and Scopus databases in February 2024. This review included only randomized controlled trials (RCTs) that assessed serum calcium levels or UCE in patients using PPIs compared to non-PPI users. Subgroup statistical analyses with hemodialysis patients, standard- or double-dose, and short- or long-term PPI use were performed. A meta-regression model was conducted with PPI treatment duration as the independent variable. Treatment effects were compared using Standardized Mean Difference (SMD) with 95% confidence intervals (CI).
Results: Of the 815 studies initially identified, 8 RCTs (n = 376) evaluated serum calcium and 3 (n = 122) evaluated UCE. PPI users had no statistically significant difference in serum calcium compared to non-PPI users (SMD -0.13; 95% CI -0.38 to 0.12; p = 0.29; I2 = 17%). Subgroup analyses with patients on hemodialysis (SMD -0.19; 95% CI -0.44 to 0.06; p = 0.14; I2 = 4%), non-hemodialysis (SMD -0.09; 95% CI -0.62 to 0.45; p = 0.76; I2 = 38%), standard-dose PPI (SMD -0.17; 95% CI -0.57 to 0.23; p = 0.41; I2 = 27%), double-dose PPI (SMD -0.11; 95% CI -0.47 to 0.24; p = 0.54; I2 = 28%), and long-term PPI users (SMD 0.03; 95% CI -0.29 to 0.34; p = 0.87; I2 = 34%) also showed no significant differences for serum calcium. Non-PPI users had a slightly higher serum calcium than short-term PPI users (SMD -0.43; 95% CI -0.80 to -0.05; p = 0.03; I2 = 0%). Meta-regression analysis showed a tendency towards higher serum calcium in patients with longer PPI treatment duration (R² = 1; p = 0.009) (Figure 1). There was no statistically significant difference regarding UCE (SMD -2.23; 95% CI -5.73 to 1.28; p = 0.21; I2 = 90%).
Discussion: PPI use was not associated with decreased serum calcium levels. Any hypothesized changes in intestinal calcium absorption, if present, are not reflected in serum calcium. Furthermore, UCE, a key compensatory mechanism affected by parathormone remains unchanged. This data raises mechanistic plausibility questions to the hypothesized noxious effect of PPIs on bone density and fracture risk.
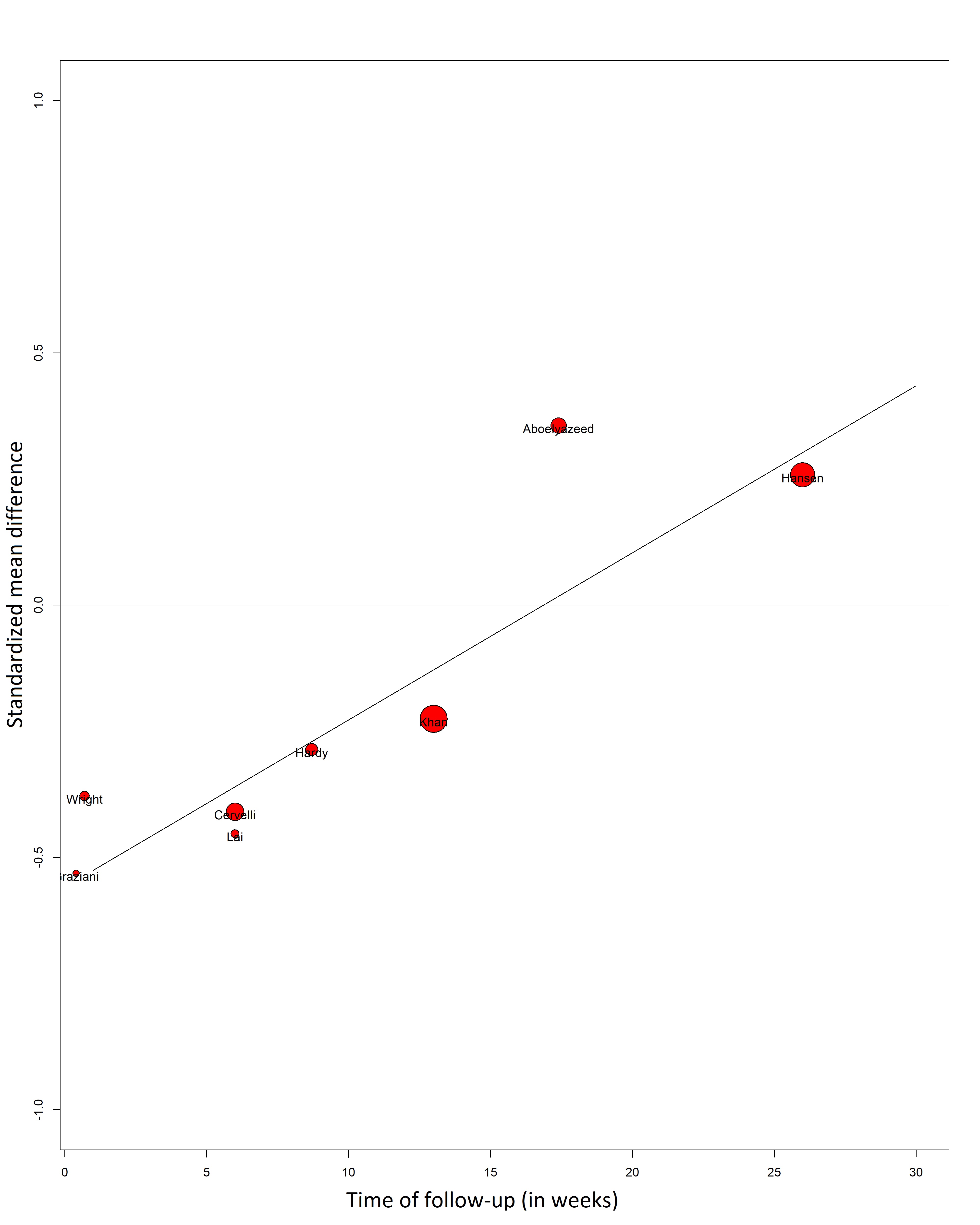
Figure: Figure 1. Meta-regression analysis showed a tendency towards higher serum calcium levels in patients with longer PPI treatment duration.
Disclosures:
Tulio L Correa indicated no relevant financial relationships.
Vanio Antunes indicated no relevant financial relationships.
Matheus V Fernandes indicated no relevant financial relationships.
Otavio C Martins indicated no relevant financial relationships.
Natalia J Milioli indicated no relevant financial relationships.
Cynthia Florencio De Mesquita indicated no relevant financial relationships.
Stefano Baraldo indicated no relevant financial relationships.
Marco Noriega indicated no relevant financial relationships.
Javier A Villafuerte-Galvez indicated no relevant financial relationships.
Tulio L Correa, MD1, Vanio Antunes, MS2, Matheus V Fernandes, MHS, MD2, Otavio C Martins, MS3, Natalia J Milioli, MD4, Cynthia Florencio De Mesquita, MS5, Stefano Baraldo, MD6, Marco Noriega, MD, MPH7, Javier A Villafuerte-Galvez, MD1. P3315 - Long-Term PPI Therapy Does Not Reduce Serum Calcium Levels: A Meta-Regression Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
