Monday Poster Session
Category: Stomach
P3316 - Low Compliance With Current Best Practice Guidelines in the Treatment and Eradication Testing of Helicobacter pylori Infections in an Academic Medical Center
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- AN
Aida Nasirishargh, MD
University of California Davis Health
Presenting Author(s)
Monica Ou, MD1, Aida Nasirishargh, MD2, Shannon Schroeder, MD1, Mili Parikh, MD3, Sili Fan, MSc1, Juan Carlos Garcia, MD1, Asha Cogdill, MD1
1University of California Davis Medical Center, Sacramento, CA; 2University of California Davis Health, Sacramento, CA; 3University of California Davis Health Graduate Medical Education, Sacramento, CA
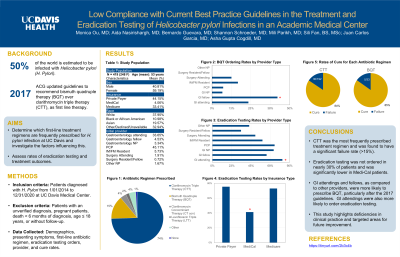
Introduction: Helicobacter pylori (HP) is believed to have infected over 50% of the world’s population. With rising macrolide antibiotic resistance rates, the American College of Gastroenterology guidelines in 2017 recommended bismuth quadruple therapy (BQT) as first-line over clarithromycin triple therapy (CTT). In addition, to ensure adequate treatment, post-treatment eradication testing was strongly recommended. Our study examines compliance with these guidelines and treatment outcomes amongst different provider training levels and departments in an academic center.
Methods: Patients diagnosed with HP from 1/01/2014 to 12/31/2020 at UC Davis Medical Center were included. Patients with an unverified diagnosis, pregnant patients, death < 6 months of diagnosis, age ≤ 18 years, and without follow-up were excluded. Demographics, presenting symptoms, first-line antibiotic regimen, eradication testing orders, provider type, and cure rates were obtained.
Results: Of 787 patients, 419 (248 F, mean age 53) met inclusion criteria. There were no differences in sex, race, age, or insurance between patients prescribed different antibiotics. CTT was prescribed more often (74%) than BQT (14%). GI attendings (23%) and fellows (42%) prescribed BQT more often than PCPs (7%) [p=0.00002]. After the 2017 guidelines, BQT was prescribed more often [26% vs. 2.8%, p=0.00001], while CTT was given less often [58% vs 90%, p=0.00001]. CTT and BQT had similar rates of cure [162 (84%) vs 28 (85%)] though the overall number of patients treated with BQT was low. Eradication testing was only ordered in 71% of patients, most often as a stool antigen (78%). When ordered, there were no differences in sex, race, or age. Patients with private insurance (75%) or Medicare (73%) were ordered testing more often than those with Medi-Cal (41%) [p=0.013]. GI attendings (81%) were most likely to order eradication testing compared to PCPs (72%), GI NPs (71%), GI fellows (63%), Surgery Attendings (50%), Surgery Residents (33%), and IM residents (58%) [p=0.01].
Discussion: CTT was the most frequently prescribed treatment and was found to have a significant failure rate ( >15%). Eradication testing was not ordered in nearly 30% of patients and was significantly lower in Medi-Cal patients. GI specialists, as compared to other providers, were more likely to order eradication testing and prescribe BQT, particularly after publication of the 2017 guidelines. This study highlights deficiencies in clinical practice and identifies areas for future education.
Disclosures:
Monica Ou, MD1, Aida Nasirishargh, MD2, Shannon Schroeder, MD1, Mili Parikh, MD3, Sili Fan, MSc1, Juan Carlos Garcia, MD1, Asha Cogdill, MD1. P3316 - Low Compliance With Current Best Practice Guidelines in the Treatment and Eradication Testing of Helicobacter pylori Infections in an Academic Medical Center, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of California Davis Medical Center, Sacramento, CA; 2University of California Davis Health, Sacramento, CA; 3University of California Davis Health Graduate Medical Education, Sacramento, CA
Introduction: Helicobacter pylori (HP) is believed to have infected over 50% of the world’s population. With rising macrolide antibiotic resistance rates, the American College of Gastroenterology guidelines in 2017 recommended bismuth quadruple therapy (BQT) as first-line over clarithromycin triple therapy (CTT). In addition, to ensure adequate treatment, post-treatment eradication testing was strongly recommended. Our study examines compliance with these guidelines and treatment outcomes amongst different provider training levels and departments in an academic center.
Methods: Patients diagnosed with HP from 1/01/2014 to 12/31/2020 at UC Davis Medical Center were included. Patients with an unverified diagnosis, pregnant patients, death < 6 months of diagnosis, age ≤ 18 years, and without follow-up were excluded. Demographics, presenting symptoms, first-line antibiotic regimen, eradication testing orders, provider type, and cure rates were obtained.
Results: Of 787 patients, 419 (248 F, mean age 53) met inclusion criteria. There were no differences in sex, race, age, or insurance between patients prescribed different antibiotics. CTT was prescribed more often (74%) than BQT (14%). GI attendings (23%) and fellows (42%) prescribed BQT more often than PCPs (7%) [p=0.00002]. After the 2017 guidelines, BQT was prescribed more often [26% vs. 2.8%, p=0.00001], while CTT was given less often [58% vs 90%, p=0.00001]. CTT and BQT had similar rates of cure [162 (84%) vs 28 (85%)] though the overall number of patients treated with BQT was low. Eradication testing was only ordered in 71% of patients, most often as a stool antigen (78%). When ordered, there were no differences in sex, race, or age. Patients with private insurance (75%) or Medicare (73%) were ordered testing more often than those with Medi-Cal (41%) [p=0.013]. GI attendings (81%) were most likely to order eradication testing compared to PCPs (72%), GI NPs (71%), GI fellows (63%), Surgery Attendings (50%), Surgery Residents (33%), and IM residents (58%) [p=0.01].
Discussion: CTT was the most frequently prescribed treatment and was found to have a significant failure rate ( >15%). Eradication testing was not ordered in nearly 30% of patients and was significantly lower in Medi-Cal patients. GI specialists, as compared to other providers, were more likely to order eradication testing and prescribe BQT, particularly after publication of the 2017 guidelines. This study highlights deficiencies in clinical practice and identifies areas for future education.
Disclosures:
Monica Ou indicated no relevant financial relationships.
Aida Nasirishargh indicated no relevant financial relationships.
Shannon Schroeder indicated no relevant financial relationships.
Mili Parikh indicated no relevant financial relationships.
Sili Fan indicated no relevant financial relationships.
Juan Carlos Garcia indicated no relevant financial relationships.
Asha Cogdill indicated no relevant financial relationships.
Monica Ou, MD1, Aida Nasirishargh, MD2, Shannon Schroeder, MD1, Mili Parikh, MD3, Sili Fan, MSc1, Juan Carlos Garcia, MD1, Asha Cogdill, MD1. P3316 - Low Compliance With Current Best Practice Guidelines in the Treatment and Eradication Testing of Helicobacter pylori Infections in an Academic Medical Center, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
