Monday Poster Session
Category: Stomach
P3322 - Factors Associated With Positive Helicobacter pylori on Repeat Endoscopy With Gastric Biopsies After an Initial Negative Test
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Anusha Agarwal, MD
Cleveland Clinic Foundation
Cleveland, OH
Presenting Author(s)
Anusha Agarwal, MD1, Arjun Chatterjee, MD1, Joyce Loh, MD2, Benjamin Click, MD3, Qijun Yang, MS4, Carol Rouphael, MD5
1Cleveland Clinic Foundation, Cleveland, OH; 2Loyola University Medical Center, Maywood, IL; 3University of Colorado, Aurora, CO; 4Cleveland Clinic, Cleveland, OH; 5Digestive Disease Institute, Cleveland Clinic, Cleveland, OH
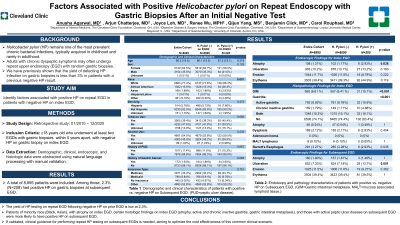
Introduction: Helicobacter pylori (HP) is typically acquired in childhood and remains one of the most prevalent chronic bacterial infections. Adults with chronic dyspeptic symptoms may often undergo repeat upper endoscopy (EGD) with random gastric biopsies. We have previously shown that the yield of detecting HP infection on gastric biopsies is less than 3% in patients with a previous negative HP result. This study aimed to identify factors associated with positive HP on repeat EGD in patients with negative HP test on index EGD.
Methods: In this retrospective study, patients ≥18 years old who underwent at least two EGDs at a large US tertiary center between 2010 and 2020 were considered and only those with negative HP on index EGD were included. EGD1 was defined as index EGD and EGD2 as first subsequent EGD during this period. Demographic, clinical, endoscopic, and histologic data were abstracted using natural language processing with manual validation. Data were summarized as mean and standard deviation for continuous variables, and percentages for categorical ones. Variables were compared by HP test results using Chi-square, Fisher exact, and two-sample t-tests. A p-value of < 0.05 was considered significant.
Results: A total of 8,895 patients were included. Among those, 2.3% (N=208) had positive HP on gastric biopsies at EGD2. In the entire cohort, mean age was 66.2±15.5 years. 64.5% were female and 77.4% were White. 47.6% were lifetime nonsmokers and 45% with no alcohol use. Factors associated with positive HP on EGD2 included Black (26.3% vs 15.3%, p=0.001) and Asian (2.93% vs 1.86%, p=0.001) race, endoscopic impression of atrophy on EGD1 (2.93% vs 1.17%, p=0.038), gastric intestinal metaplasia (15.1% vs. 6.41%, p< 0.001), active gastritis (15.6% vs 8.76%, p< 0.001), chronic inactive gastritis (4.88% vs. 1.71%, p< 0.001) on pathology from EGD1, or endoscopic impression of ulceration (13.7% vs 7.18%, p=0.001) on EGD2. There was no difference in HP yield at EGD2 among those with or without antibiotics or proton pump inhibitors prescribed prior to EGD (Table 1).
Discussion: The yield of HP testing on repeat EGD following negative HP on prior EGD is low. Higher risk features for positive HP include minority race, certain histologic findings on index exam, and those with active peptic ulcer disease on subsequent exam. If validated, clinical guidance for performing repeat HP testing on subsequent EGDs is needed, aiming to optimize the cost effectiveness of this common clinical scenario.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Anusha Agarwal, MD1, Arjun Chatterjee, MD1, Joyce Loh, MD2, Benjamin Click, MD3, Qijun Yang, MS4, Carol Rouphael, MD5. P3322 - Factors Associated With Positive <i>Helicobacter pylori</i> on Repeat Endoscopy With Gastric Biopsies After an Initial Negative Test, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Cleveland Clinic Foundation, Cleveland, OH; 2Loyola University Medical Center, Maywood, IL; 3University of Colorado, Aurora, CO; 4Cleveland Clinic, Cleveland, OH; 5Digestive Disease Institute, Cleveland Clinic, Cleveland, OH
Introduction: Helicobacter pylori (HP) is typically acquired in childhood and remains one of the most prevalent chronic bacterial infections. Adults with chronic dyspeptic symptoms may often undergo repeat upper endoscopy (EGD) with random gastric biopsies. We have previously shown that the yield of detecting HP infection on gastric biopsies is less than 3% in patients with a previous negative HP result. This study aimed to identify factors associated with positive HP on repeat EGD in patients with negative HP test on index EGD.
Methods: In this retrospective study, patients ≥18 years old who underwent at least two EGDs at a large US tertiary center between 2010 and 2020 were considered and only those with negative HP on index EGD were included. EGD1 was defined as index EGD and EGD2 as first subsequent EGD during this period. Demographic, clinical, endoscopic, and histologic data were abstracted using natural language processing with manual validation. Data were summarized as mean and standard deviation for continuous variables, and percentages for categorical ones. Variables were compared by HP test results using Chi-square, Fisher exact, and two-sample t-tests. A p-value of < 0.05 was considered significant.
Results: A total of 8,895 patients were included. Among those, 2.3% (N=208) had positive HP on gastric biopsies at EGD2. In the entire cohort, mean age was 66.2±15.5 years. 64.5% were female and 77.4% were White. 47.6% were lifetime nonsmokers and 45% with no alcohol use. Factors associated with positive HP on EGD2 included Black (26.3% vs 15.3%, p=0.001) and Asian (2.93% vs 1.86%, p=0.001) race, endoscopic impression of atrophy on EGD1 (2.93% vs 1.17%, p=0.038), gastric intestinal metaplasia (15.1% vs. 6.41%, p< 0.001), active gastritis (15.6% vs 8.76%, p< 0.001), chronic inactive gastritis (4.88% vs. 1.71%, p< 0.001) on pathology from EGD1, or endoscopic impression of ulceration (13.7% vs 7.18%, p=0.001) on EGD2. There was no difference in HP yield at EGD2 among those with or without antibiotics or proton pump inhibitors prescribed prior to EGD (Table 1).
Discussion: The yield of HP testing on repeat EGD following negative HP on prior EGD is low. Higher risk features for positive HP include minority race, certain histologic findings on index exam, and those with active peptic ulcer disease on subsequent exam. If validated, clinical guidance for performing repeat HP testing on subsequent EGDs is needed, aiming to optimize the cost effectiveness of this common clinical scenario.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Anusha Agarwal indicated no relevant financial relationships.
Arjun Chatterjee indicated no relevant financial relationships.
Joyce Loh indicated no relevant financial relationships.
Benjamin Click: AbbVie – Consultant. BMS – Consultant. Janssen – Consultant. Pfizer – Consultant. Prometheus – Consultant. Takeda – Consultant. TARGET-RWE – Consultant.
Qijun Yang indicated no relevant financial relationships.
Carol Rouphael indicated no relevant financial relationships.
Anusha Agarwal, MD1, Arjun Chatterjee, MD1, Joyce Loh, MD2, Benjamin Click, MD3, Qijun Yang, MS4, Carol Rouphael, MD5. P3322 - Factors Associated With Positive <i>Helicobacter pylori</i> on Repeat Endoscopy With Gastric Biopsies After an Initial Negative Test, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
