Monday Poster Session
Category: Stomach
P3329 - Helicobacter pylori-Negative MALT Lymphoma Presenting With Severe Gastrointestinal Bleeding: Insights from a Systematic Review of Published Case Reports
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Ana P. Rivera Arauz, MD
Nassau University Medical Center
Amityville, NY
Presenting Author(s)
Ana P. Rivera, MD1, James R. Pellegrini, MD2, Tulika Saggar, MD3, Atul Sinha, MD3, Sandra Gomez, MD3, Paul Mustacchia, MD, MBA3
1Nassau University Medical Center, Amityville, NY; 2Nassau University Medical Center, Great River, NY; 3Nassau University Medical Center, East Meadow, NY
Introduction: Gastric mucosa-associated lymphoid tissue (MALT) lymphoma usually has an indolent course. Life-threatening GI bleeding in H. pylori-negative gastric MALT lymphoma is rare and poorly documented. In this study, we explore the distinctive clinical presentation and management of H. pylori-negative MALT lymphoma presenting with severe GI bleeding. We sought to better understand the findings, interventions, and outcomes in patients diagnosed with this entity.
Methods: We searched Google Scholar, PubMed, and ScienceDirect from January 2019 to the present. Search words included "Helicobacter Pylori Negative MALT" and "GI bleeding." Data on demographics, history of GI disorders, clinical presentation of GI bleeding, EGD findings, intervention for GI bleeding, treatment of MALT lymphoma, and outcomes were collected.
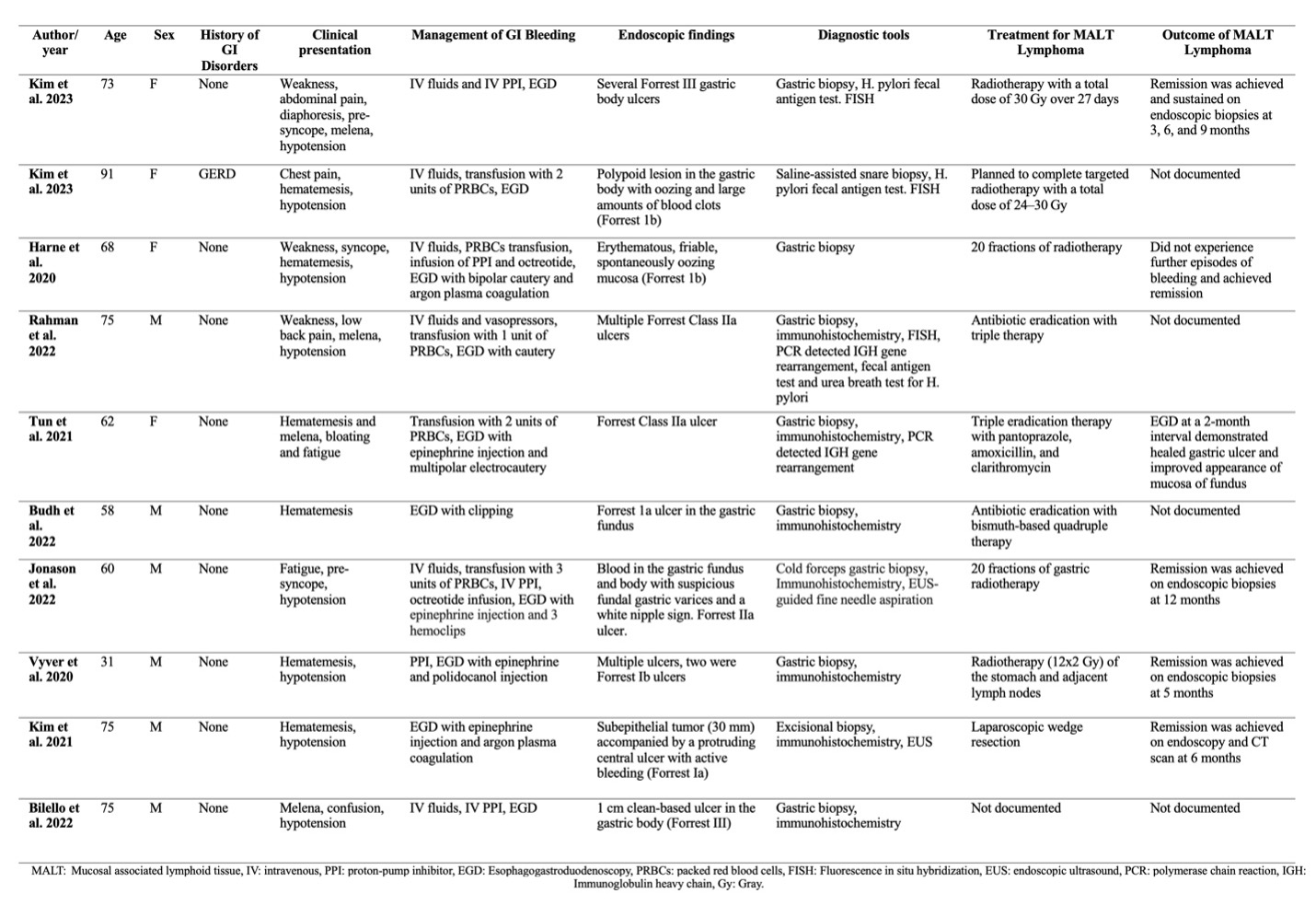
Results: We identified 10 case reports of H. pylori-negative MALT lymphoma with severe GI bleeding. The cohort included six men and four women, average age 66.8 years, mostly without prior GI disorders. Most (80%) experienced hypovolemic shock. Bleeding was hematemesis (50%), melena (30%), or both (10%), with 10% occult bleeding. Mean admission hemoglobin was 8.7 g/dL; half required transfusions, and 10% needed pressor support. EGD showed ulcerative patterns (80%) and mixed exophytic-ulcerative lesions (20%). Forrest 1b and IIa ulcers were common (30% each), followed by Forrest Ia and III (20% each). Epinephrine injection, combined with other interventions, was the preferred hemostasis approach (40%). Diagnosis was confirmed via biopsy in all cases, with 100% H. pylori negativity. Other tests included FISH, PCR for IGH gene rearrangement, and EUS. Most common treatment was radiotherapy (50%); 30% received antibiotics, and one underwent laparoscopic resection.
Discussion: Our study highlights the uncommon occurrence of severe gastrointestinal bleeding in H. pylori-negative MALT lymphoma. Unlike H. pylori-positive cases, where eradication therapy is well-established, the management of H. pylori-negative cases remains challenging and underexplored. While current guidelines advocate radiation therapy as the preferred treatment, emerging evidence suggests potential benefits from H. pylori eradication therapy even in negative cases. This raises important questions about optimizing treatment approaches and stresses the need for further clinical research to validate these findings and develop tailored management protocols for H. pylori-negative MALT lymphoma presenting with severe GI bleeding.
Disclosures:
Ana P. Rivera, MD1, James R. Pellegrini, MD2, Tulika Saggar, MD3, Atul Sinha, MD3, Sandra Gomez, MD3, Paul Mustacchia, MD, MBA3. P3329 - Helicobacter pylori-Negative MALT Lymphoma Presenting With Severe Gastrointestinal Bleeding: Insights from a Systematic Review of Published Case Reports, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Nassau University Medical Center, Amityville, NY; 2Nassau University Medical Center, Great River, NY; 3Nassau University Medical Center, East Meadow, NY
Introduction: Gastric mucosa-associated lymphoid tissue (MALT) lymphoma usually has an indolent course. Life-threatening GI bleeding in H. pylori-negative gastric MALT lymphoma is rare and poorly documented. In this study, we explore the distinctive clinical presentation and management of H. pylori-negative MALT lymphoma presenting with severe GI bleeding. We sought to better understand the findings, interventions, and outcomes in patients diagnosed with this entity.
Methods: We searched Google Scholar, PubMed, and ScienceDirect from January 2019 to the present. Search words included "Helicobacter Pylori Negative MALT" and "GI bleeding." Data on demographics, history of GI disorders, clinical presentation of GI bleeding, EGD findings, intervention for GI bleeding, treatment of MALT lymphoma, and outcomes were collected.
Results: We identified 10 case reports of H. pylori-negative MALT lymphoma with severe GI bleeding. The cohort included six men and four women, average age 66.8 years, mostly without prior GI disorders. Most (80%) experienced hypovolemic shock. Bleeding was hematemesis (50%), melena (30%), or both (10%), with 10% occult bleeding. Mean admission hemoglobin was 8.7 g/dL; half required transfusions, and 10% needed pressor support. EGD showed ulcerative patterns (80%) and mixed exophytic-ulcerative lesions (20%). Forrest 1b and IIa ulcers were common (30% each), followed by Forrest Ia and III (20% each). Epinephrine injection, combined with other interventions, was the preferred hemostasis approach (40%). Diagnosis was confirmed via biopsy in all cases, with 100% H. pylori negativity. Other tests included FISH, PCR for IGH gene rearrangement, and EUS. Most common treatment was radiotherapy (50%); 30% received antibiotics, and one underwent laparoscopic resection.
Discussion: Our study highlights the uncommon occurrence of severe gastrointestinal bleeding in H. pylori-negative MALT lymphoma. Unlike H. pylori-positive cases, where eradication therapy is well-established, the management of H. pylori-negative cases remains challenging and underexplored. While current guidelines advocate radiation therapy as the preferred treatment, emerging evidence suggests potential benefits from H. pylori eradication therapy even in negative cases. This raises important questions about optimizing treatment approaches and stresses the need for further clinical research to validate these findings and develop tailored management protocols for H. pylori-negative MALT lymphoma presenting with severe GI bleeding.
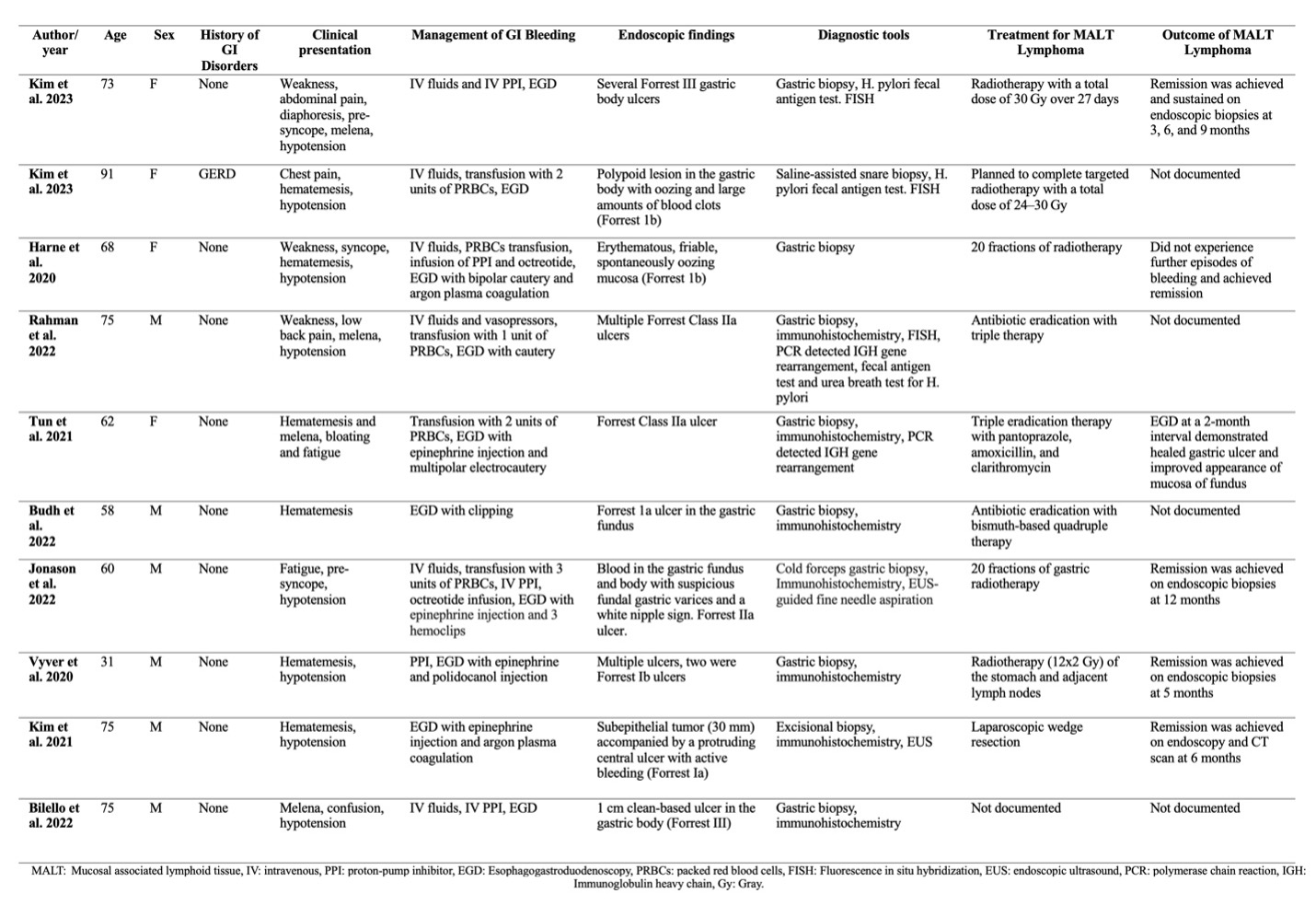
Figure: Table 1. Helicobacter pylori-negative MALT lymphoma and severe gastrointestinal bleeding cases.
Disclosures:
Ana Rivera indicated no relevant financial relationships.
James Pellegrini indicated no relevant financial relationships.
Tulika Saggar indicated no relevant financial relationships.
Atul Sinha indicated no relevant financial relationships.
Sandra Gomez indicated no relevant financial relationships.
Paul Mustacchia indicated no relevant financial relationships.
Ana P. Rivera, MD1, James R. Pellegrini, MD2, Tulika Saggar, MD3, Atul Sinha, MD3, Sandra Gomez, MD3, Paul Mustacchia, MD, MBA3. P3329 - Helicobacter pylori-Negative MALT Lymphoma Presenting With Severe Gastrointestinal Bleeding: Insights from a Systematic Review of Published Case Reports, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
