Monday Poster Session
Category: Stomach
P3339 - Addressing an Emerging Clinical Need: Nasal Metoclopramide's Impact on Diabetic Gastroparesis in Patients Taking GLP-1 Agonists
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

David C. Kunkel, MD
University of California San Diego
La Jolla, CA
Presenting Author(s)
Award: ACG Outstanding Research Award in the Stomach Category
Award: Presidential Poster Award
David C. Kunkel, MD1, Richard W. McCallum, MD2, Christopher Quesenberry, BSc3, Mostafa Shokoohi, PhD4, Paul Spin, PhD4, Michael Cline, DO5
1University of California San Diego, La Jolla, CA; 2Texas Tech University Health Sciences Center School of Medicine, El Paso, TX; 3Evoke Pharma, Phoenix, AZ; 4Eversana, Burlington, ON, Canada; 5Cleveland Clinic Foundation, Cleveland, OH
Introduction: Diabetic gastroparesis (DGP) is a chronic upper gastrointestinal disorder characterized by delayed gastric emptying without mechanical obstruction, causing nausea, vomiting, and abdominal pain. GLP-1 agonists, used to treat type 2 diabetes, can exacerbate these symptoms by delaying gastric emptying. This study compares healthcare resource utilization (HRU) in DGP patients treated with nasal (NMCP) vs. oral metoclopramide (OMCP) with recent GLP-1 agonist use.
Methods: A retrospective, matched cohort of NMCP- and OMCP-treated patients (257 per group) was derived from specialty pharmacy data and the Symphony Integrated Dataverse, an open claims database. Adult patients with a DGP diagnosis and ≥6 months pre- and post-index (treatment initiation) continuous data were included. Propensity score matching reduced imbalances in age, region, payor, Charlson Comorbidity Score, and 6-month pre-index hospitalization/emergency department (ED) use. Patients with a GLP-1 prescription filled ≤6 months pre-index were analyzed. Post-treatment all-cause and DGP-related HRU (gastroparesis, nausea, vomiting) were compared using a multivariable negative binomial regression model, with results as conditional incident rate ratios (cIRR) and 95% confidence intervals (CI).
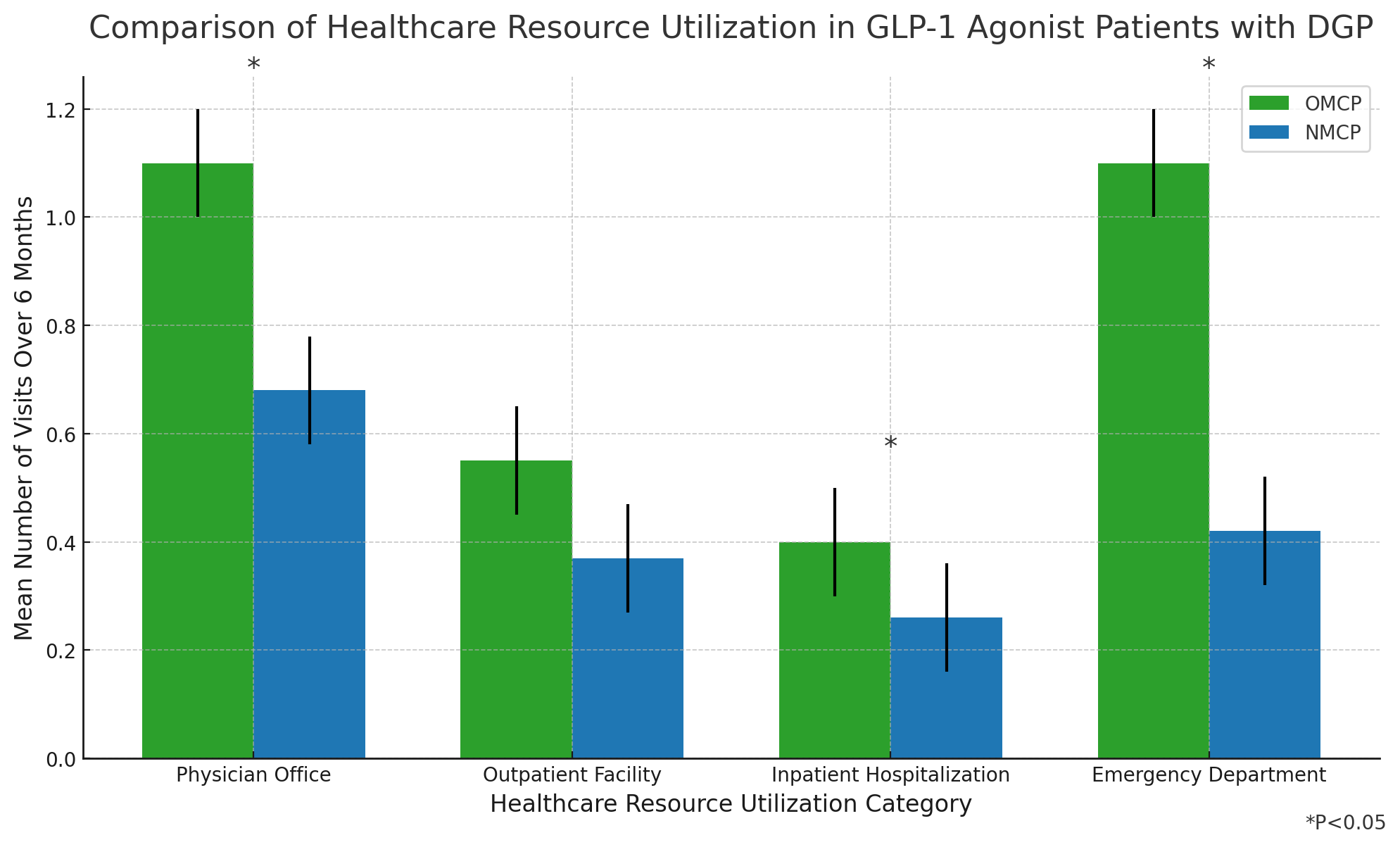
Results: The subgroup included 51 NMCP and 41 OMCP patients with a prior GLP-1 prescription. NMCP patients were slightly older (55.1 vs. 53.1 years) and had more pre-index hospitalization/ED admissions (31.4% vs. 19.5%). For NMCP patients, all-cause ED visits decreased by 55% (mean [SD]: 0.25 [1.13] post-index vs. 0.55 [1.30] pre-index; P=0.063) and DGP-related ED visits decreased by 28% (mean [SD]: 0.18 [0.99] post-index vs. 0.25 [1.28] pre-index; P=0.203).
All-cause and DGP-related ED visits were 91% lower (cIRR: 0.09, 95% CI: 0.01, 0.42; P=0.001) and 89% lower (cIRR: 0.11, 95% CI: 0, 0.93; P=0.046) for NMCP vs. OMCP. Furthermore, all-cause and DGP-related office visits were 41% lower (cIRR: 0.59, 95% CI: 0.37, 0.94; P=0.027) and 66% lower (cIRR: 0.34, 95% CI: 0.017, 0.65; P=0.001) for NMCP vs. OMCP. All-cause clinic, outpatient, and inpatient visits showed similar trends favoring NMCP vs. OMCP.
Discussion: In DGP patients with a prior claim for GLP-1, NMCP use was associated with numerically and significantly reduced all-cause and DGP-related HRU compared to pre-treatment utilization and OMCP-treated controls.
Disclosures:
David C. Kunkel, MD1, Richard W. McCallum, MD2, Christopher Quesenberry, BSc3, Mostafa Shokoohi, PhD4, Paul Spin, PhD4, Michael Cline, DO5. P3339 - Addressing an Emerging Clinical Need: Nasal Metoclopramide's Impact on Diabetic Gastroparesis in Patients Taking GLP-1 Agonists, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Award: Presidential Poster Award
David C. Kunkel, MD1, Richard W. McCallum, MD2, Christopher Quesenberry, BSc3, Mostafa Shokoohi, PhD4, Paul Spin, PhD4, Michael Cline, DO5
1University of California San Diego, La Jolla, CA; 2Texas Tech University Health Sciences Center School of Medicine, El Paso, TX; 3Evoke Pharma, Phoenix, AZ; 4Eversana, Burlington, ON, Canada; 5Cleveland Clinic Foundation, Cleveland, OH
Introduction: Diabetic gastroparesis (DGP) is a chronic upper gastrointestinal disorder characterized by delayed gastric emptying without mechanical obstruction, causing nausea, vomiting, and abdominal pain. GLP-1 agonists, used to treat type 2 diabetes, can exacerbate these symptoms by delaying gastric emptying. This study compares healthcare resource utilization (HRU) in DGP patients treated with nasal (NMCP) vs. oral metoclopramide (OMCP) with recent GLP-1 agonist use.
Methods: A retrospective, matched cohort of NMCP- and OMCP-treated patients (257 per group) was derived from specialty pharmacy data and the Symphony Integrated Dataverse, an open claims database. Adult patients with a DGP diagnosis and ≥6 months pre- and post-index (treatment initiation) continuous data were included. Propensity score matching reduced imbalances in age, region, payor, Charlson Comorbidity Score, and 6-month pre-index hospitalization/emergency department (ED) use. Patients with a GLP-1 prescription filled ≤6 months pre-index were analyzed. Post-treatment all-cause and DGP-related HRU (gastroparesis, nausea, vomiting) were compared using a multivariable negative binomial regression model, with results as conditional incident rate ratios (cIRR) and 95% confidence intervals (CI).
Results: The subgroup included 51 NMCP and 41 OMCP patients with a prior GLP-1 prescription. NMCP patients were slightly older (55.1 vs. 53.1 years) and had more pre-index hospitalization/ED admissions (31.4% vs. 19.5%). For NMCP patients, all-cause ED visits decreased by 55% (mean [SD]: 0.25 [1.13] post-index vs. 0.55 [1.30] pre-index; P=0.063) and DGP-related ED visits decreased by 28% (mean [SD]: 0.18 [0.99] post-index vs. 0.25 [1.28] pre-index; P=0.203).
All-cause and DGP-related ED visits were 91% lower (cIRR: 0.09, 95% CI: 0.01, 0.42; P=0.001) and 89% lower (cIRR: 0.11, 95% CI: 0, 0.93; P=0.046) for NMCP vs. OMCP. Furthermore, all-cause and DGP-related office visits were 41% lower (cIRR: 0.59, 95% CI: 0.37, 0.94; P=0.027) and 66% lower (cIRR: 0.34, 95% CI: 0.017, 0.65; P=0.001) for NMCP vs. OMCP. All-cause clinic, outpatient, and inpatient visits showed similar trends favoring NMCP vs. OMCP.
Discussion: In DGP patients with a prior claim for GLP-1, NMCP use was associated with numerically and significantly reduced all-cause and DGP-related HRU compared to pre-treatment utilization and OMCP-treated controls.
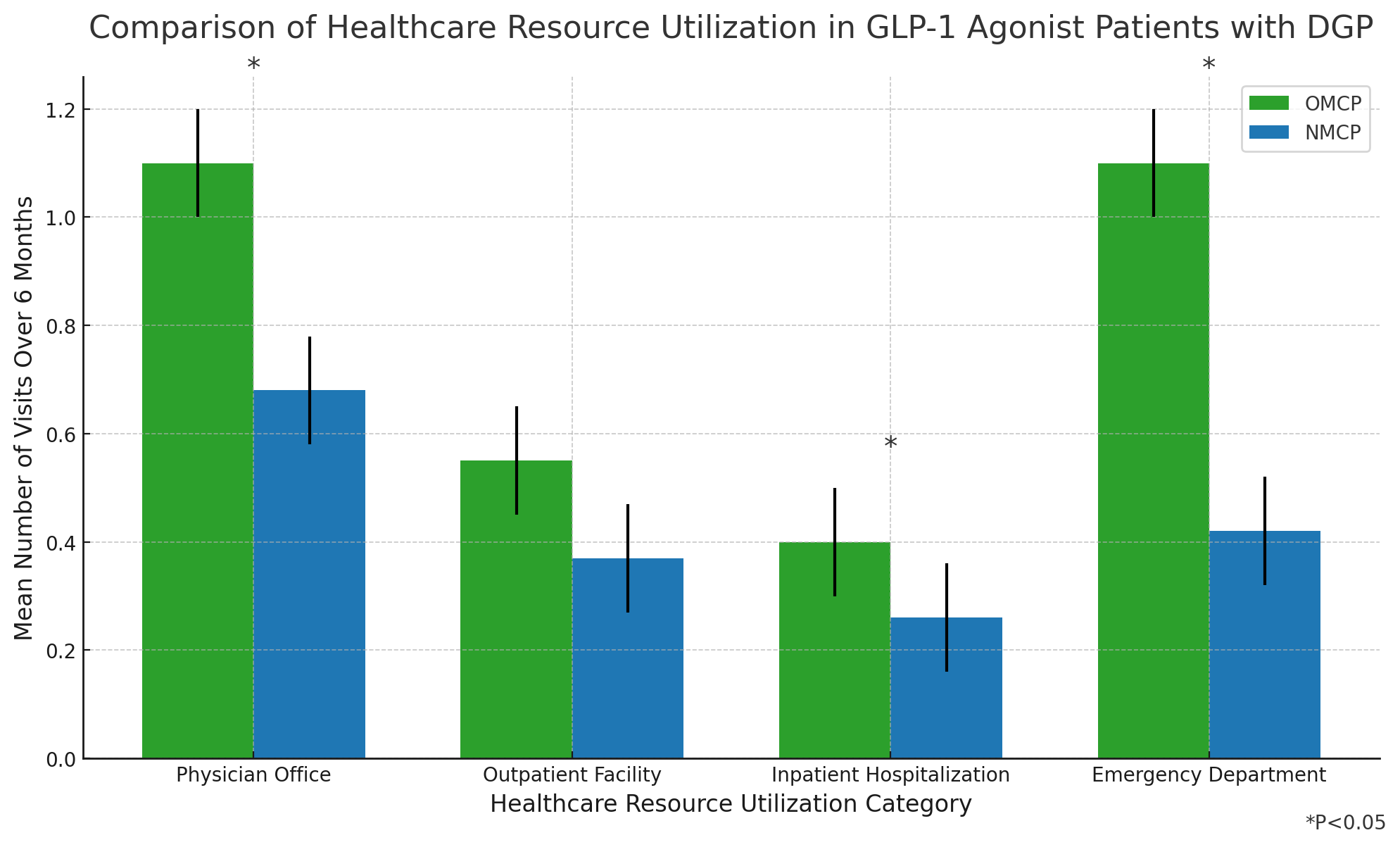
Figure: Figure 1: Comparison of Healthcare Resource Utilization in GLP-1 Agonist Patients with Diabetic Gastroparesis
Disclosures:
David Kunkel: Evoke Pharma – Consultant. Phathom Pharmaceuticals – Speakers Bureau. Regeneron Pharmaceuticals – Speakers Bureau. Sanofi – Speakers Bureau. Vanda Pharmaceuticals – Grant/Research Support.
Richard McCallum: Evoke Pharma – Consultant.
Christopher Quesenberry: Evoke Pharma – Employee.
Mostafa Shokoohi: Eversana – Employee.
Paul Spin: Eversana – Employee.
Michael Cline indicated no relevant financial relationships.
David C. Kunkel, MD1, Richard W. McCallum, MD2, Christopher Quesenberry, BSc3, Mostafa Shokoohi, PhD4, Paul Spin, PhD4, Michael Cline, DO5. P3339 - Addressing an Emerging Clinical Need: Nasal Metoclopramide's Impact on Diabetic Gastroparesis in Patients Taking GLP-1 Agonists, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

