Monday Poster Session
Category: Stomach
P3340 - Gastric Phytobezoars as a Consequence of Chronic Afferent Loop Syndrome
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Scarlet Louis-Jean, MD, MBA, MSAN
Luminis Health Anne Arundel Medical Center
Annapolis, MD
Presenting Author(s)
Scarlet Louis-Jean, MD, MBA, MSAN1, Ripple Mehta, MD2, Joseph Jennings, MD2
1Luminis Health Anne Arundel Medical Center, Annapolis, MD; 2MedStar Georgetown University Hospital, Washington, DC
Introduction: Bezoars are concretions of indigestible or inedible material, which are commonly found in the stomach. There are 4 types of bezoars including phytobezoars (indigestible food particles), trichobezoars (hair and food particles), lactobezoar (milk protein conglomerates), and pharmacobezoars (medication concretions), of which phytobezoars account for 40% of all reported cases. Formation of these aggregates is often precipitated by altered gastrointestinal anatomy and/or motility, such as afferent loop syndrome, which is often seen following procedures involving anastomosis of the stomach or esophagus to the jejunum.
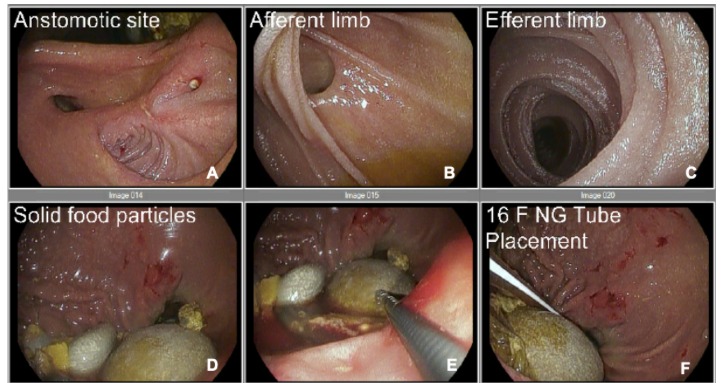
Case Description/Methods: An 81-year-old woman with a history of chemoradiation, pancreatic head adenocarcinoma status-post Whipple’s procedure, gastrectomy and gastrojejunostomy, with multiple failed esophagoduodenoscopy balloon dilations, and upper gastrointestinal bleed from a GJ anastomotic marginal ulcer presented to the emergency department for worsening 2-year history of intermittent abdominal spasms, bloating, and early satiety. On EGD she was found to have several large bezoars, which were too large and compact for snare removal or fragmentation, respectively. She underwent gastrectomy with surgical resection of the previous GJ en-bloc, which was found to contain several large bezoars. The remaining stomach was drained, and a Roux-en-Y gastrojejunostomy with new jejunojejunostomy into the pancreaticobiliary limb of the previous Whipple reconstruction was created. On discharge, the patient exhibited normal bowel and urinary habits, and satisfactory pain control.
Discussion: Non-invasive treatment options of bezoars are often preferred, with the first-line options being mechanical disintegration (e.g., electrosurgical knife, mechanical lithotripter, laser destruction) or consumption of chemical solvents (e.g., sodium bicarbonate, hydrochloric acid, Coca-Cola lavage) followed by endoscopy for fragmentation and snare removal. Surgery is often reserved for patients who do not respond to minimally invasive options, have persistent symptoms, and anatomical disturbances such as strictures. Due to the patient’s GJ stricture and numerous prohibitively large bezoars that were difficult to endoscopically retrieve, surgery was determined to be the preferred option to reduce the likelihood of recurrence. However, despite preventive measures the recurrence rate is reportedly 13.5% in patients with gastrectomy, although no data exists for surgical revisions.
Disclosures:
Scarlet Louis-Jean, MD, MBA, MSAN1, Ripple Mehta, MD2, Joseph Jennings, MD2. P3340 - Gastric Phytobezoars as a Consequence of Chronic Afferent Loop Syndrome, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Luminis Health Anne Arundel Medical Center, Annapolis, MD; 2MedStar Georgetown University Hospital, Washington, DC
Introduction: Bezoars are concretions of indigestible or inedible material, which are commonly found in the stomach. There are 4 types of bezoars including phytobezoars (indigestible food particles), trichobezoars (hair and food particles), lactobezoar (milk protein conglomerates), and pharmacobezoars (medication concretions), of which phytobezoars account for 40% of all reported cases. Formation of these aggregates is often precipitated by altered gastrointestinal anatomy and/or motility, such as afferent loop syndrome, which is often seen following procedures involving anastomosis of the stomach or esophagus to the jejunum.
Case Description/Methods: An 81-year-old woman with a history of chemoradiation, pancreatic head adenocarcinoma status-post Whipple’s procedure, gastrectomy and gastrojejunostomy, with multiple failed esophagoduodenoscopy balloon dilations, and upper gastrointestinal bleed from a GJ anastomotic marginal ulcer presented to the emergency department for worsening 2-year history of intermittent abdominal spasms, bloating, and early satiety. On EGD she was found to have several large bezoars, which were too large and compact for snare removal or fragmentation, respectively. She underwent gastrectomy with surgical resection of the previous GJ en-bloc, which was found to contain several large bezoars. The remaining stomach was drained, and a Roux-en-Y gastrojejunostomy with new jejunojejunostomy into the pancreaticobiliary limb of the previous Whipple reconstruction was created. On discharge, the patient exhibited normal bowel and urinary habits, and satisfactory pain control.
Discussion: Non-invasive treatment options of bezoars are often preferred, with the first-line options being mechanical disintegration (e.g., electrosurgical knife, mechanical lithotripter, laser destruction) or consumption of chemical solvents (e.g., sodium bicarbonate, hydrochloric acid, Coca-Cola lavage) followed by endoscopy for fragmentation and snare removal. Surgery is often reserved for patients who do not respond to minimally invasive options, have persistent symptoms, and anatomical disturbances such as strictures. Due to the patient’s GJ stricture and numerous prohibitively large bezoars that were difficult to endoscopically retrieve, surgery was determined to be the preferred option to reduce the likelihood of recurrence. However, despite preventive measures the recurrence rate is reportedly 13.5% in patients with gastrectomy, although no data exists for surgical revisions.
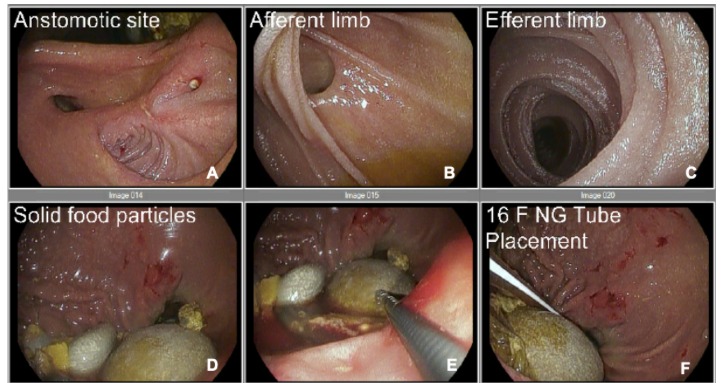
Figure: Endoscopic imaging of the gastric body demonstrating the site of anastomosis (A), afferent limb (B), efferent limb (C), solid food particles (D, E, F).
Disclosures:
Scarlet Louis-Jean indicated no relevant financial relationships.
Ripple Mehta indicated no relevant financial relationships.
Joseph Jennings indicated no relevant financial relationships.
Scarlet Louis-Jean, MD, MBA, MSAN1, Ripple Mehta, MD2, Joseph Jennings, MD2. P3340 - Gastric Phytobezoars as a Consequence of Chronic Afferent Loop Syndrome, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
