Monday Poster Session
Category: Stomach
P3381 - Phlegmonous Gastritis Due to Presumed Helicobacter pylori Infection
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- ST
Sangini Tolia, MD
Trinity Health Ann Arbor Hospital
Ann Arbor, MI
Presenting Author(s)
Sangini Tolia, MD1, Marjan Haider, MD1, Sarvani Surapaneni, MD1, Kevin Platt, MD2, Emily Tommolino, MD2
1Trinity Health Ann Arbor Hospital, Ann Arbor, MI; 2Huron Gastroenterology, Ann Arbor, MI
Introduction: Phlegmonous or purulent gastritis (PG) is a rare infection of the gastric wall. Patients may present with nonspecific symptoms and can develop rapid systemic progression with high mortality. Here, we present a case of acute PG that initially did not respond to antibiotic therapy and was empirically treated with quadruple therapy for presumed Helicobacter pylori infection. The patient recovered and did not need surgery.
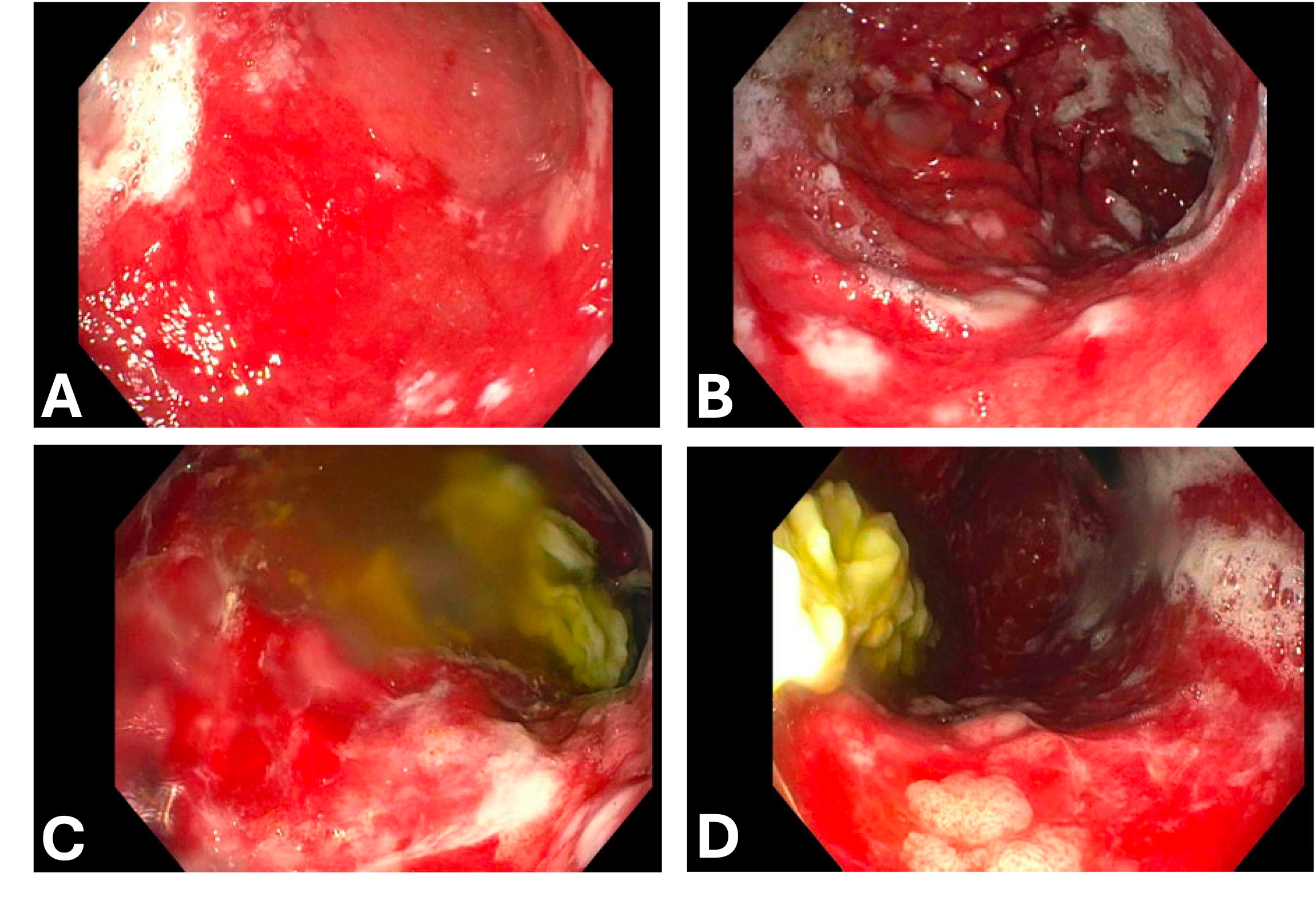
Case Description/Methods: A 59-year-old female presented to the hospital with two days of intractable nausea, vomiting, epigastric pain, and inability to tolerate oral intake. She endorsed chronic constipation, and denied diarrhea, fever, chills, sick contacts, and had not eaten any unusual foods. She had no pertinent medical or family history. Home medications included a daily proton-pump inhibitor (PPI). Her leukocyte count was 20.2 × 109/L (normal 4-10). Abdominal computed tomography (CT) was notable for diffuse gastric wall thickening. An upper gastrointestinal endoscopy (EGD) showed severe, unusual appearing mucosa with antral sparing. Biopsy revealed diffuse acute purulent gastritis with surface ulceration and erosion, crypt abscesses and pockets of neutrophils. It was negative for Helicobacter pylori, fungal organisms, virocytes, and malignancy. She was initially treated with ceftriaxone and twice daily intravenous proton-pump inhibitor. However, due to persistent symptoms and leukocytosis, a second EGD was performed, showing persistent acute gastritis with intense erythema and exudates in the gastric fundus and body, with an abrupt transition to normal-appearing mucosa in the antrum. She was taking a PPI prior to the biopsy, so we considered the possibility of a false negative H. pylori result. She was then empirically started on quadruple therapy (clarithromycin, metronidazole, amoxicillin, and PPI) for 14 days to treat H. pylori. At her follow-up appointment, her symptoms and leukocytosis had improved. She was scheduled for a repeat outpatient EGD to ensure endoscopic resolution.
Discussion: PG is a rare diagnosis characterized by pus and inflammation of the gastric submucosa. The most common causative pathogens are Streptococci, and antibiotics are the initial treatment of choice. In our case, no infection was isolated from the biopsies, but she improved after starting empiric treatment for H. pylori. PG carries a high mortality of up to 84%, so it is crucial to identify the diagnosis and treat promptly. If medical therapy fails, surgical intervention may be required.
Disclosures:
Sangini Tolia, MD1, Marjan Haider, MD1, Sarvani Surapaneni, MD1, Kevin Platt, MD2, Emily Tommolino, MD2. P3381 - Phlegmonous Gastritis Due to Presumed <i>Helicobacter pylori</i> Infection, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Trinity Health Ann Arbor Hospital, Ann Arbor, MI; 2Huron Gastroenterology, Ann Arbor, MI
Introduction: Phlegmonous or purulent gastritis (PG) is a rare infection of the gastric wall. Patients may present with nonspecific symptoms and can develop rapid systemic progression with high mortality. Here, we present a case of acute PG that initially did not respond to antibiotic therapy and was empirically treated with quadruple therapy for presumed Helicobacter pylori infection. The patient recovered and did not need surgery.
Case Description/Methods: A 59-year-old female presented to the hospital with two days of intractable nausea, vomiting, epigastric pain, and inability to tolerate oral intake. She endorsed chronic constipation, and denied diarrhea, fever, chills, sick contacts, and had not eaten any unusual foods. She had no pertinent medical or family history. Home medications included a daily proton-pump inhibitor (PPI). Her leukocyte count was 20.2 × 109/L (normal 4-10). Abdominal computed tomography (CT) was notable for diffuse gastric wall thickening. An upper gastrointestinal endoscopy (EGD) showed severe, unusual appearing mucosa with antral sparing. Biopsy revealed diffuse acute purulent gastritis with surface ulceration and erosion, crypt abscesses and pockets of neutrophils. It was negative for Helicobacter pylori, fungal organisms, virocytes, and malignancy. She was initially treated with ceftriaxone and twice daily intravenous proton-pump inhibitor. However, due to persistent symptoms and leukocytosis, a second EGD was performed, showing persistent acute gastritis with intense erythema and exudates in the gastric fundus and body, with an abrupt transition to normal-appearing mucosa in the antrum. She was taking a PPI prior to the biopsy, so we considered the possibility of a false negative H. pylori result. She was then empirically started on quadruple therapy (clarithromycin, metronidazole, amoxicillin, and PPI) for 14 days to treat H. pylori. At her follow-up appointment, her symptoms and leukocytosis had improved. She was scheduled for a repeat outpatient EGD to ensure endoscopic resolution.
Discussion: PG is a rare diagnosis characterized by pus and inflammation of the gastric submucosa. The most common causative pathogens are Streptococci, and antibiotics are the initial treatment of choice. In our case, no infection was isolated from the biopsies, but she improved after starting empiric treatment for H. pylori. PG carries a high mortality of up to 84%, so it is crucial to identify the diagnosis and treat promptly. If medical therapy fails, surgical intervention may be required.
Figure: A - First EGD. Severe erythema in the gastric body
B - First EGD. Exudates in the gastric body
C and D - Second EGD. Persistent erythema and inflammation in the gastric body
B - First EGD. Exudates in the gastric body
C and D - Second EGD. Persistent erythema and inflammation in the gastric body
Disclosures:
Sangini Tolia indicated no relevant financial relationships.
Marjan Haider indicated no relevant financial relationships.
Sarvani Surapaneni indicated no relevant financial relationships.
Kevin Platt indicated no relevant financial relationships.
Emily Tommolino indicated no relevant financial relationships.
Sangini Tolia, MD1, Marjan Haider, MD1, Sarvani Surapaneni, MD1, Kevin Platt, MD2, Emily Tommolino, MD2. P3381 - Phlegmonous Gastritis Due to Presumed <i>Helicobacter pylori</i> Infection, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
