Monday Poster Session
Category: Stomach
P3390 - A Rare Case of Non-pylori Helicobacter Gastritis from Feline Mouth-to-Mouth CPR
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Alex Chang, MD
Donald and Barbara Zucker School of Medicine at Hofstra/Northwell North Shore and Long Island Jewish University Hospital
Irvine, CA
Presenting Author(s)
Alex Chang, MD1, Allan Schuss, MD2, Leonard Stein, MD2
1Donald and Barbara Zucker School of Medicine at Hofstra/Northwell North Shore and Long Island Jewish University Hospital, Irvine, CA; 2Gastroenterology Associates of Uniondale, Uniondale, NY
Introduction: Non-H. pylori species are a rare cause of gastritis in humans. A clinical history indicating possible inoculation from feline species should raise suspicion of infection with zoonotic Helicobacter species such as H. heilmannii.
Case Description/Methods: A 57-year old woman presented with two-weeks of epigastric pain. At the onset of the symptoms, she visited the ED where she was discharged on PPIs.
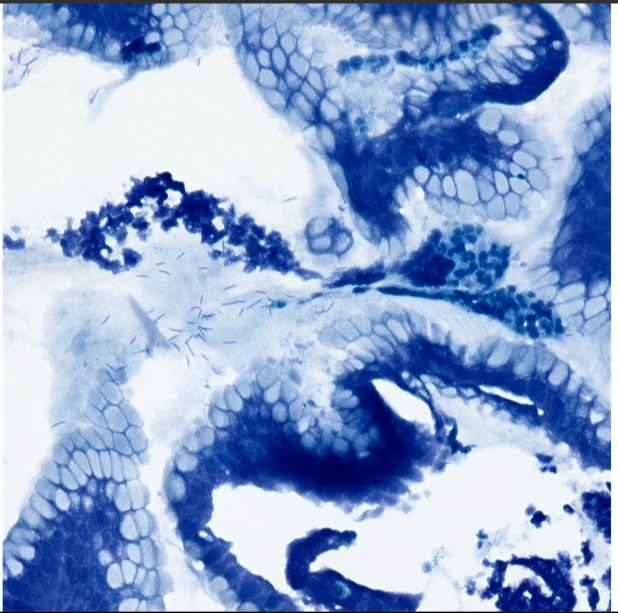
The patient underwent an EGD, which revealed patchy inflammation as well as a 7-mm ulcer in the gastric antrum. Histological examination showed mild active gastritis, but no evidence of H. pylori. The patient was prescribed daily PPI therapy. 2 months later, repeat EGD demonstrated diffuse severe inflammatory changes throughout the gastric antrum. Biopsy revealed severe active gastritis. A Diff-Quik stain was positive for Helicobacter species larger and more tightly coiled than H. pylori, consistent with H. heilmannii, a common organism found in the stomachs of cats (Figure 1). At follow-up, the patient revealed having 3 pet cats at home and that 10 days before onset of epigastric pain, she had performed mouth-to-mouth CPR on a cat.
Treatment of the patient consisted of a 2-week triple therapy regimen typically used for treatment of H. pylori (lansoprazole, amoxicillin, and clarithromycin). On repeat EGD, the gastric mucosa was normal and biopsy revealed minimal inactive gastritis. Diff-quik stain was negative for any organisms. Clinically, the patient reported feeling asymptomatic.
Discussion: H. heilmanii can cause gastritis in humans. In most case reports, patients have long-term contact with cats. In the current case, the patient was a long-term cat owner, but given the acute onset of symptoms after performing CPR on her cat, there is reasonable suspicion that mouth-to-mouth CPR may have been an inoculating event.
Interestingly, initial EGD, while demonstrating gastritis, did not show evidence of organisms. Possible explanations include use of PPI masking inflammation or a shorter incubation period from time of exposure, leading to lower counts of H. heilmanii.
Importantly, the current case reinforces that H. heilmanii may be suspected in patients with no clear etiology of gastritis and a history of exposure to cats. Prior literature indicates that due to weaker urease activity, H. heilmanii gastritis may yield a negative breath test so EGD with biopsy may be useful in patients with clinical suspicion. Treatment with similar regimens for H. pylori appears effective in eradicating H. heilmanii.
Disclosures:
Alex Chang, MD1, Allan Schuss, MD2, Leonard Stein, MD2. P3390 - A Rare Case of Non-<i>pylori Helicobacter</i> Gastritis from Feline Mouth-to-Mouth CPR, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Donald and Barbara Zucker School of Medicine at Hofstra/Northwell North Shore and Long Island Jewish University Hospital, Irvine, CA; 2Gastroenterology Associates of Uniondale, Uniondale, NY
Introduction: Non-H. pylori species are a rare cause of gastritis in humans. A clinical history indicating possible inoculation from feline species should raise suspicion of infection with zoonotic Helicobacter species such as H. heilmannii.
Case Description/Methods: A 57-year old woman presented with two-weeks of epigastric pain. At the onset of the symptoms, she visited the ED where she was discharged on PPIs.
The patient underwent an EGD, which revealed patchy inflammation as well as a 7-mm ulcer in the gastric antrum. Histological examination showed mild active gastritis, but no evidence of H. pylori. The patient was prescribed daily PPI therapy. 2 months later, repeat EGD demonstrated diffuse severe inflammatory changes throughout the gastric antrum. Biopsy revealed severe active gastritis. A Diff-Quik stain was positive for Helicobacter species larger and more tightly coiled than H. pylori, consistent with H. heilmannii, a common organism found in the stomachs of cats (Figure 1). At follow-up, the patient revealed having 3 pet cats at home and that 10 days before onset of epigastric pain, she had performed mouth-to-mouth CPR on a cat.
Treatment of the patient consisted of a 2-week triple therapy regimen typically used for treatment of H. pylori (lansoprazole, amoxicillin, and clarithromycin). On repeat EGD, the gastric mucosa was normal and biopsy revealed minimal inactive gastritis. Diff-quik stain was negative for any organisms. Clinically, the patient reported feeling asymptomatic.
Discussion: H. heilmanii can cause gastritis in humans. In most case reports, patients have long-term contact with cats. In the current case, the patient was a long-term cat owner, but given the acute onset of symptoms after performing CPR on her cat, there is reasonable suspicion that mouth-to-mouth CPR may have been an inoculating event.
Interestingly, initial EGD, while demonstrating gastritis, did not show evidence of organisms. Possible explanations include use of PPI masking inflammation or a shorter incubation period from time of exposure, leading to lower counts of H. heilmanii.
Importantly, the current case reinforces that H. heilmanii may be suspected in patients with no clear etiology of gastritis and a history of exposure to cats. Prior literature indicates that due to weaker urease activity, H. heilmanii gastritis may yield a negative breath test so EGD with biopsy may be useful in patients with clinical suspicion. Treatment with similar regimens for H. pylori appears effective in eradicating H. heilmanii.
Figure: Diff-Quick stain showing numerous spiraled-shaped microorganisms consistent with H. heilmannii (400x)
Disclosures:
Alex Chang indicated no relevant financial relationships.
Allan Schuss indicated no relevant financial relationships.
Leonard Stein indicated no relevant financial relationships.
Alex Chang, MD1, Allan Schuss, MD2, Leonard Stein, MD2. P3390 - A Rare Case of Non-<i>pylori Helicobacter</i> Gastritis from Feline Mouth-to-Mouth CPR, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
