Monday Poster Session
Category: Stomach
P3416 - When Nivolumab Turns Nasty: A Rare Case of Hemorrhagic Gastritis
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Franklin Liu, MD
Banner - University of Arizona
Tucson, AZ
Presenting Author(s)
Award: Presidential Poster Award
Brandon Witten, MD1, Franklin Liu, MD2, Samuel H. Cheong, DO2, Diane Rodden, MD1, Demaretta Rush, MD1, Joshua Melson, MD1
1University of Arizona College of Medicine, Tucson, AZ; 2Banner - University of Arizona, Tucson, AZ
Introduction: Nivolumab, an immune checkpoint inhibitor targeting PD-1, has revolutionized the treatment of various cancers, especially metastatic melanoma. While generally well-tolerated, nivolumab can cause immune related adverse events (irAE) by enhancing the immune response of regulatory T cells. Gastrointestinal toxicity is one of the more frequent irAEs and usually presents as colitis. Although gastritis has been reported, it is rare.
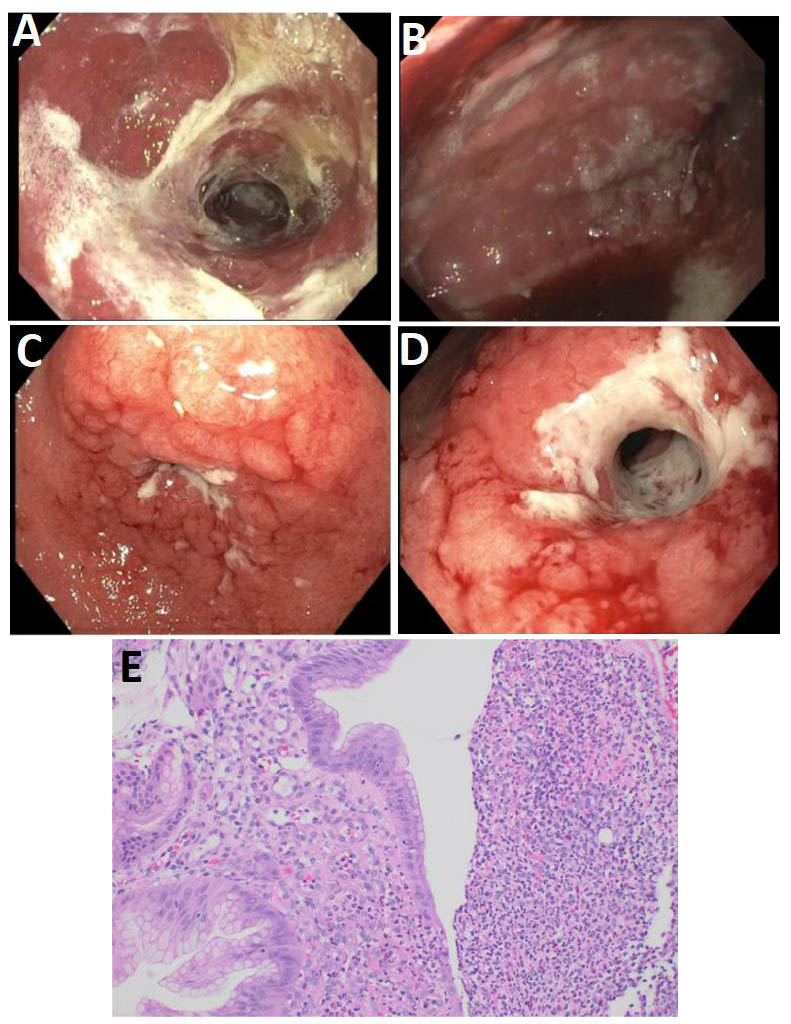
Case Description/Methods: 47 year old female with a history of metastatic melanoma was initially started on combination ipilumumab/nivolumab immunotherapy, later transitioned to nivolumab monotherapy by oncology after experiencing grade 3 hepatitis. She was referred to GI for evaluation of 2 months of nausea, dysphagia, and acid reflux. PET scan showed diffuse gastric uptake, EGD was significant for severe and diffuse erythematous mucosa with overlying exudate in the entire stomach.
Biopsies showed acute ulcerative gastritis. Infectious workup was negative including H. pylori, CMV, HSV 1/2 immunostains, and GMS stain and there was no evidence of intestinal metaplasia. SOX10 and TCK immunostains were negative for atypical cells and infiltrating epithelial cells, respectively, ruling out malignancy. The most likely diagnosis was thought to be grade 3 immune checkpoint inhibitor induced (ICI) gastritis.
After irAE was confirmed prednisone 40mg daily, sucralfate and omeprazole 20mg twice daily was started. Nivolumab was held and a steroid taper (decreasing 5mg per week) began once symptoms improved. After completion of the steroid taper repeat EGD still showed severe inflammation, erosions, erythema, and friability in the entire stomach. Biopsies again showed acute ulcerative gastritis.
Although her symptoms had improved, given ongoing extensive gastritis on EGD and a concern for refractory ICI gastritis despite high dose steroids, the plan was to initiate infliximab therapy. Unfortunately, infliximab was not started due to insurance approval delays. She continued to be off therapy (except for omeprazole) for two months and was now asymptomatic. A final third EGD was done to re-stage her gastritis. EGD with biopsies at this time showed complete resolution and no evidence of active inflammation.
Discussion: This case underscores the importance of recognizing nivolumab-induced hemorrhagic gastritis, an uncommon irAE. Early identification, cessation of the drug along with timely intervention with immunosuppressive therapy and supportive care can significantly improve outcomes.
Disclosures:
Brandon Witten, MD1, Franklin Liu, MD2, Samuel H. Cheong, DO2, Diane Rodden, MD1, Demaretta Rush, MD1, Joshua Melson, MD1. P3416 - When Nivolumab Turns Nasty: A Rare Case of Hemorrhagic Gastritis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Brandon Witten, MD1, Franklin Liu, MD2, Samuel H. Cheong, DO2, Diane Rodden, MD1, Demaretta Rush, MD1, Joshua Melson, MD1
1University of Arizona College of Medicine, Tucson, AZ; 2Banner - University of Arizona, Tucson, AZ
Introduction: Nivolumab, an immune checkpoint inhibitor targeting PD-1, has revolutionized the treatment of various cancers, especially metastatic melanoma. While generally well-tolerated, nivolumab can cause immune related adverse events (irAE) by enhancing the immune response of regulatory T cells. Gastrointestinal toxicity is one of the more frequent irAEs and usually presents as colitis. Although gastritis has been reported, it is rare.
Case Description/Methods: 47 year old female with a history of metastatic melanoma was initially started on combination ipilumumab/nivolumab immunotherapy, later transitioned to nivolumab monotherapy by oncology after experiencing grade 3 hepatitis. She was referred to GI for evaluation of 2 months of nausea, dysphagia, and acid reflux. PET scan showed diffuse gastric uptake, EGD was significant for severe and diffuse erythematous mucosa with overlying exudate in the entire stomach.
Biopsies showed acute ulcerative gastritis. Infectious workup was negative including H. pylori, CMV, HSV 1/2 immunostains, and GMS stain and there was no evidence of intestinal metaplasia. SOX10 and TCK immunostains were negative for atypical cells and infiltrating epithelial cells, respectively, ruling out malignancy. The most likely diagnosis was thought to be grade 3 immune checkpoint inhibitor induced (ICI) gastritis.
After irAE was confirmed prednisone 40mg daily, sucralfate and omeprazole 20mg twice daily was started. Nivolumab was held and a steroid taper (decreasing 5mg per week) began once symptoms improved. After completion of the steroid taper repeat EGD still showed severe inflammation, erosions, erythema, and friability in the entire stomach. Biopsies again showed acute ulcerative gastritis.
Although her symptoms had improved, given ongoing extensive gastritis on EGD and a concern for refractory ICI gastritis despite high dose steroids, the plan was to initiate infliximab therapy. Unfortunately, infliximab was not started due to insurance approval delays. She continued to be off therapy (except for omeprazole) for two months and was now asymptomatic. A final third EGD was done to re-stage her gastritis. EGD with biopsies at this time showed complete resolution and no evidence of active inflammation.
Discussion: This case underscores the importance of recognizing nivolumab-induced hemorrhagic gastritis, an uncommon irAE. Early identification, cessation of the drug along with timely intervention with immunosuppressive therapy and supportive care can significantly improve outcomes.
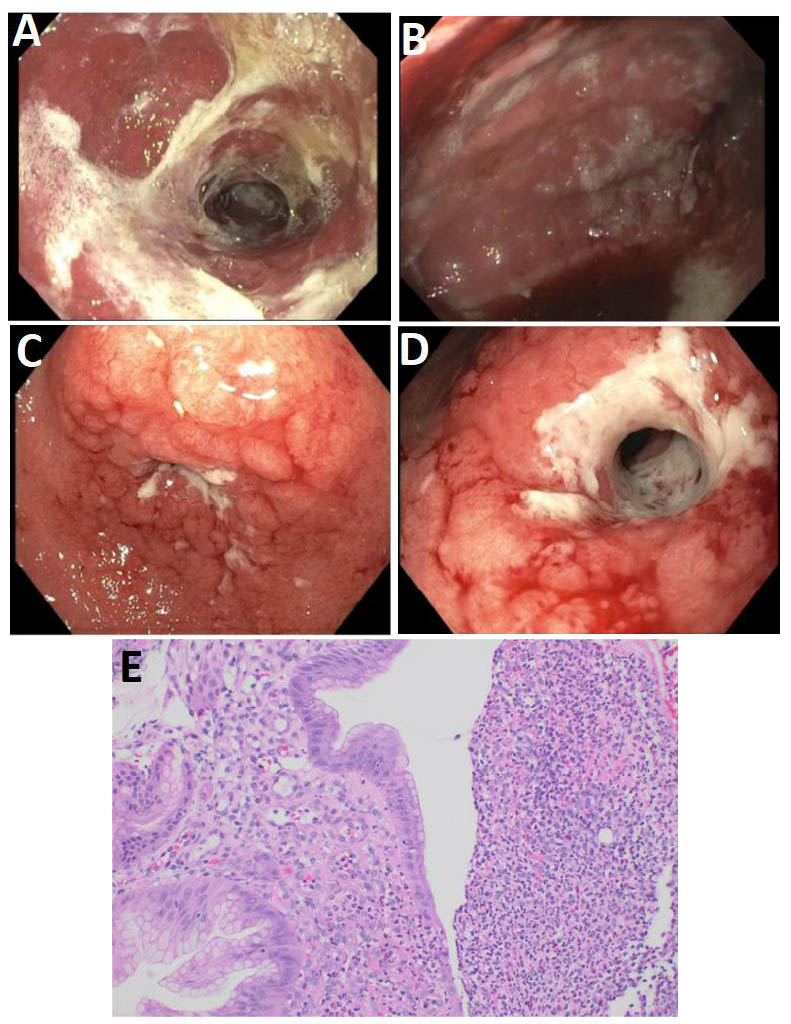
Figure: A: First EGD showing the gastric antrum with severe gastritis with overlying exudate.
B: First EGD displaying the gastric body with severe gastritis.
C: Second EGD showing persistent severe inflammation near the duodenal bulb.
D: Second EGD focusing on the pre-pyloric stomach still displaying persistent severe inflammation and confluent ulcerations.
E: 20X magnification of gastric biopsy neutrophilic infiltration can be seen in the gastric epithelium and lamina propria adjacent to the ulceration.
B: First EGD displaying the gastric body with severe gastritis.
C: Second EGD showing persistent severe inflammation near the duodenal bulb.
D: Second EGD focusing on the pre-pyloric stomach still displaying persistent severe inflammation and confluent ulcerations.
E: 20X magnification of gastric biopsy neutrophilic infiltration can be seen in the gastric epithelium and lamina propria adjacent to the ulceration.
Disclosures:
Brandon Witten indicated no relevant financial relationships.
Franklin Liu indicated no relevant financial relationships.
Samuel Cheong indicated no relevant financial relationships.
Diane Rodden indicated no relevant financial relationships.
Demaretta Rush indicated no relevant financial relationships.
Joshua Melson indicated no relevant financial relationships.
Brandon Witten, MD1, Franklin Liu, MD2, Samuel H. Cheong, DO2, Diane Rodden, MD1, Demaretta Rush, MD1, Joshua Melson, MD1. P3416 - When Nivolumab Turns Nasty: A Rare Case of Hemorrhagic Gastritis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

