Tuesday Poster Session
Category: Biliary/Pancreas
P3437 - Differential Outcomes of ERCP in Malignant and Benign Biliary Strictures: A National Inpatient Sample Analysis
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Gautam Maddineni, MD
Florida State University
Cape Coral, FL
Presenting Author(s)
Gautam Maddineni, MD1, Akram Ahmad, MBBS2, Zaid Ansari, MD3, Silpa Choday, MD4, Tilak Upendra. Shah, MD2
1Florida State University, Cape Coral, FL; 2Cleveland Clinic Florida, Weston, FL; 3Cleveland Clinic Florida, Plantation, FL; 4Creighton University School of Medicine, Phoenix, AZ
Introduction: Endoscopic retrograde cholangiopancreatography (ERCP) is essential for managing biliary and pancreatic ductal diseases. Malignant biliary strictures (MS) are often associated with pancreaticobiliary cancers and pose significant challenges. In contrast, benign biliary strictures (BS) result from chronic pancreatitis or post-surgical complications and require accurate differentiation for optimal treatment.
Methods: The research used the National Inpatient Sample database from 2016 to 2019 to compare outcomes of hospitalized adults who underwent ERCP for biliary stricture. We compared outcomes between malignant and benign biliary stricture patients using STATA 18 software and various statistical tests. All descriptive variables were analyzed through both univariate and multivariate analysis, and the results were adjusted for multiple factors, with statistical significance at p < 0.005
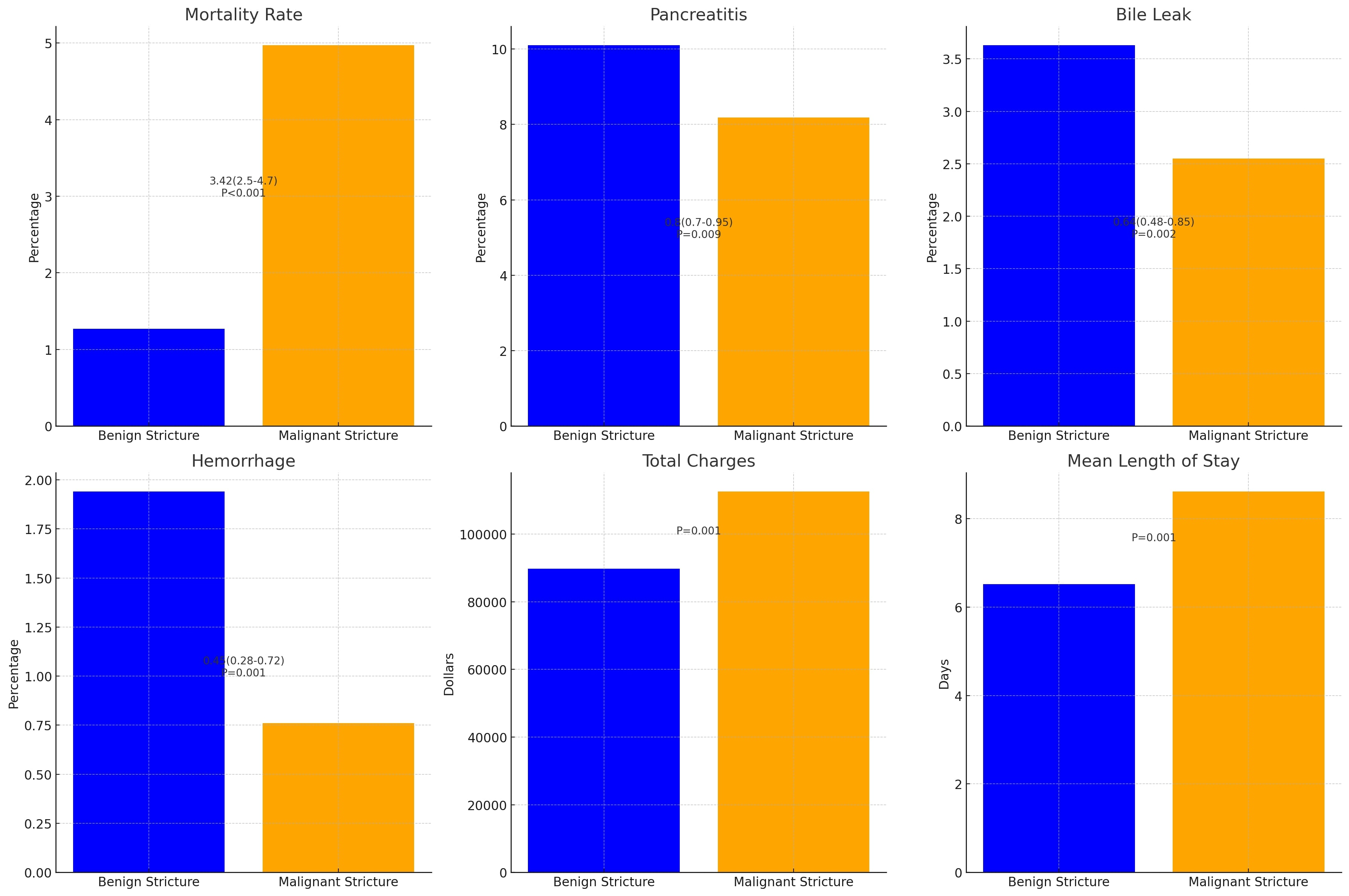
Results: Mortality rates were 2,195 (2.63%) for BS and 14,520 (6.78%) for MS, with MS having higher mortality (aOR: 4.07, p< 0.0001). Non-teaching hospitals(NTH) had higher mortality for MS (8.19% vs. 6.53%, p< 0.001), while teaching hospitals(TH) had higher mortality for BS (2.71% vs. 2.25%, p< 0.001).
ERCP for MS accounted for 1.0% (p< 0.001) of cases and 1.68% for BS (p=0.17), with more procedures in TH (67.16%, p=0.17). Post-ERCP infections occurred in 0.15%, higher in MS (0.26%, p=0.3, aOR: 1.85, p=0.25). Bile leaks were 1.21%, higher in BS (3.63%, p=0.007, aOR: 0.63, p=0.002). Pancreatitis occurred in 8.92%, more frequent in BS (10.1%, p=0.004, aOR: 0.8, p=0.009). Hemorrhage occurred in 9.04%, higher in BS (1.94%, p< 0.001, aOR: 0.45, p< 0.001).
The mean length of stay (LOS) was 4.28 days, longer for MS (8.61 days, p< 0.001, adjusted increase of 1.65 days, p< 0.001). Mean total charges were $70,463, higher for MS ($112,537 vs. $89,694, adjusted increase of $18,463, p< 0.001, R²=0.03).
Discussion: The research findings suggest that patients with MS have worse outcomes following ERCP than those with BS. Higher in-hospital mortality rates for MS, especially in NTH, highlight the complexity of managing malignant cases. Additionally, increased post-ERCP infection rates and longer LOS for MS patients emphasize the need for advanced treatment approaches. TH had better outcomes for MS but worse outcomes for BS, suggesting the need for tailored protocols. These findings underscore the critical importance of early diagnosis and specialized care in enhancing ERCP outcomes for patients with MS.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Gautam Maddineni, MD1, Akram Ahmad, MBBS2, Zaid Ansari, MD3, Silpa Choday, MD4, Tilak Upendra. Shah, MD2. P3437 - Differential Outcomes of ERCP in Malignant and Benign Biliary Strictures: A National Inpatient Sample Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Florida State University, Cape Coral, FL; 2Cleveland Clinic Florida, Weston, FL; 3Cleveland Clinic Florida, Plantation, FL; 4Creighton University School of Medicine, Phoenix, AZ
Introduction: Endoscopic retrograde cholangiopancreatography (ERCP) is essential for managing biliary and pancreatic ductal diseases. Malignant biliary strictures (MS) are often associated with pancreaticobiliary cancers and pose significant challenges. In contrast, benign biliary strictures (BS) result from chronic pancreatitis or post-surgical complications and require accurate differentiation for optimal treatment.
Methods: The research used the National Inpatient Sample database from 2016 to 2019 to compare outcomes of hospitalized adults who underwent ERCP for biliary stricture. We compared outcomes between malignant and benign biliary stricture patients using STATA 18 software and various statistical tests. All descriptive variables were analyzed through both univariate and multivariate analysis, and the results were adjusted for multiple factors, with statistical significance at p < 0.005
Results: Mortality rates were 2,195 (2.63%) for BS and 14,520 (6.78%) for MS, with MS having higher mortality (aOR: 4.07, p< 0.0001). Non-teaching hospitals(NTH) had higher mortality for MS (8.19% vs. 6.53%, p< 0.001), while teaching hospitals(TH) had higher mortality for BS (2.71% vs. 2.25%, p< 0.001).
ERCP for MS accounted for 1.0% (p< 0.001) of cases and 1.68% for BS (p=0.17), with more procedures in TH (67.16%, p=0.17). Post-ERCP infections occurred in 0.15%, higher in MS (0.26%, p=0.3, aOR: 1.85, p=0.25). Bile leaks were 1.21%, higher in BS (3.63%, p=0.007, aOR: 0.63, p=0.002). Pancreatitis occurred in 8.92%, more frequent in BS (10.1%, p=0.004, aOR: 0.8, p=0.009). Hemorrhage occurred in 9.04%, higher in BS (1.94%, p< 0.001, aOR: 0.45, p< 0.001).
The mean length of stay (LOS) was 4.28 days, longer for MS (8.61 days, p< 0.001, adjusted increase of 1.65 days, p< 0.001). Mean total charges were $70,463, higher for MS ($112,537 vs. $89,694, adjusted increase of $18,463, p< 0.001, R²=0.03).
Discussion: The research findings suggest that patients with MS have worse outcomes following ERCP than those with BS. Higher in-hospital mortality rates for MS, especially in NTH, highlight the complexity of managing malignant cases. Additionally, increased post-ERCP infection rates and longer LOS for MS patients emphasize the need for advanced treatment approaches. TH had better outcomes for MS but worse outcomes for BS, suggesting the need for tailored protocols. These findings underscore the critical importance of early diagnosis and specialized care in enhancing ERCP outcomes for patients with MS.
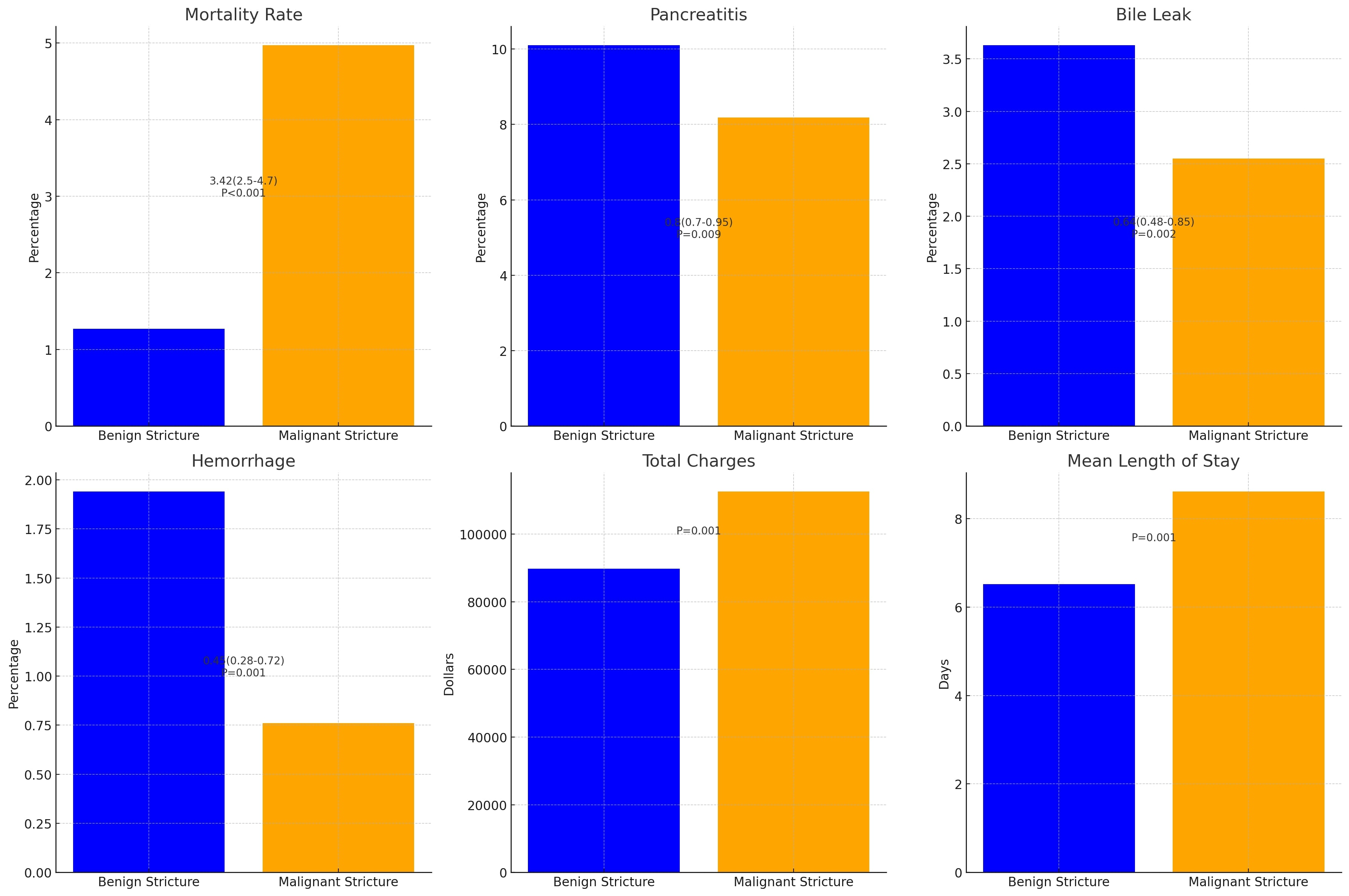
Figure: OUTCOMES: Impact of ERCP procedure on Biliary Stricture type and procedure-related Complications and Healthcare Burden
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Gautam Maddineni indicated no relevant financial relationships.
Akram Ahmad indicated no relevant financial relationships.
Zaid Ansari indicated no relevant financial relationships.
Silpa Choday indicated no relevant financial relationships.
Tilak Shah indicated no relevant financial relationships.
Gautam Maddineni, MD1, Akram Ahmad, MBBS2, Zaid Ansari, MD3, Silpa Choday, MD4, Tilak Upendra. Shah, MD2. P3437 - Differential Outcomes of ERCP in Malignant and Benign Biliary Strictures: A National Inpatient Sample Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
