Tuesday Poster Session
Category: Biliary/Pancreas
P3438 - Impact of Hospital Type on ERCP Outcomes for Biliary Strictures: A Comparative Analysis of Teaching vs Non-Teaching Hospitals (2016-2019)
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Gautam Maddineni, MD
Florida State University
Cape Coral, FL
Presenting Author(s)
Gautam Maddineni, MD1, Akram Ahmad, MBBS2, Zaid Ansari, MD3, Tilak Upendra. Shah, MD2
1Florida State University, Cape Coral, FL; 2Cleveland Clinic Florida, Weston, FL; 3Cleveland Clinic Florida, Plantation, FL
Introduction: Biliary strictures(BS) are when the bile duct narrows or becomes blocked, preventing bile from flowing from the liver to the small intestine. Previous research shows varying outcomes, with teaching hospitals(TH) having higher complication rates due to trainee involvement but better outcomes for complex procedures due to advanced expertise. This study compares ERCP outcomes and complication rates for biliary strictures in TH vs. non-teaching hospitals(NTH).
Methods: The study used the National Inpatient Sample database from 2016 to 2019 to analyze adults admitted to the hospital for biliary stricture and who underwent ERCP. Patients with choledocholithiasis were excluded to ensure the accuracy of the testing population. The analysis was performed using STATA 18 software, including t-tests, linear regression, and logistic regression tests. All descriptive variables were analyzed using univariate and multivariate analysis. Results were adjusted for various factors, with statistical significance at p < 0.005.
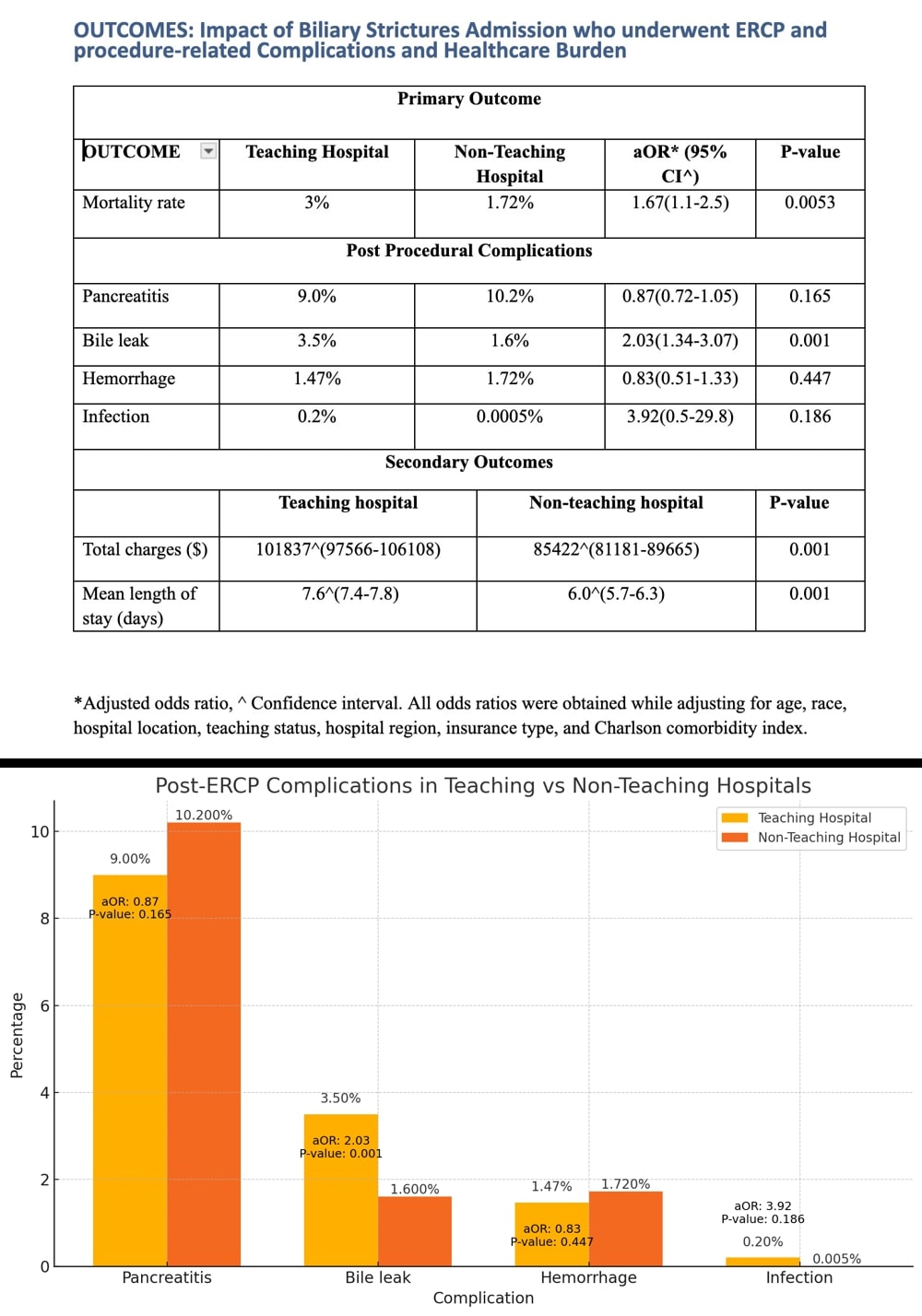
Results: The overall mortality rate was 2.72% (95% CI 2.39-3.1), with a higher rate for TH compared to NTH (3% vs 1.72%, p=0.005). BS were treated more in TH (78.5% vs. 21.5% in NTH), with a higher percentage of ERCP procedures (67.5% vs 32.5%).
Mortality increased with age (OR: 1.02, p< 0.001), was higher in Blacks (OR: 1.96, p< 0.001), and was lowest in the Midwest(OR 0.6, p=0.02). The mean length of stay for adults undergoing ERCP was 7.3 days and was 65% greater in TH when compared to NTH.
The total hospital charge on hospitalization was higher in TH at $101837(97566-106108) compared to $85422 for nonteaching. Post-procedure complications of Pancreatitis(OR: 0.87)and Hemorrhage(OR: 0.82) were lower in TH but increased in Bile Leak(OR: 2.03) and Infections(OR: 3.09) compared to NTH.
Discussion: Our study reveals that TH exhibits higher mortality rates, longer hospital stays, and greater costs for ERCP in biliary strictures, but they manage complications more effectively. Complications like pancreatitis and hemorrhage were lower in TH compared to NTH, aligning with prior studies highlighting the expertise of TH in handling complex cases. However, increased bile leaks and infections suggest areas for improvement. These findings align with existing literature emphasizing the dual-edged nature of care in teaching hospitals, where advanced expertise coexists with higher immediate risks and costs.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Gautam Maddineni, MD1, Akram Ahmad, MBBS2, Zaid Ansari, MD3, Tilak Upendra. Shah, MD2. P3438 - Impact of Hospital Type on ERCP Outcomes for Biliary Strictures: A Comparative Analysis of Teaching vs Non-Teaching Hospitals (2016-2019), ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Florida State University, Cape Coral, FL; 2Cleveland Clinic Florida, Weston, FL; 3Cleveland Clinic Florida, Plantation, FL
Introduction: Biliary strictures(BS) are when the bile duct narrows or becomes blocked, preventing bile from flowing from the liver to the small intestine. Previous research shows varying outcomes, with teaching hospitals(TH) having higher complication rates due to trainee involvement but better outcomes for complex procedures due to advanced expertise. This study compares ERCP outcomes and complication rates for biliary strictures in TH vs. non-teaching hospitals(NTH).
Methods: The study used the National Inpatient Sample database from 2016 to 2019 to analyze adults admitted to the hospital for biliary stricture and who underwent ERCP. Patients with choledocholithiasis were excluded to ensure the accuracy of the testing population. The analysis was performed using STATA 18 software, including t-tests, linear regression, and logistic regression tests. All descriptive variables were analyzed using univariate and multivariate analysis. Results were adjusted for various factors, with statistical significance at p < 0.005.
Results: The overall mortality rate was 2.72% (95% CI 2.39-3.1), with a higher rate for TH compared to NTH (3% vs 1.72%, p=0.005). BS were treated more in TH (78.5% vs. 21.5% in NTH), with a higher percentage of ERCP procedures (67.5% vs 32.5%).
Mortality increased with age (OR: 1.02, p< 0.001), was higher in Blacks (OR: 1.96, p< 0.001), and was lowest in the Midwest(OR 0.6, p=0.02). The mean length of stay for adults undergoing ERCP was 7.3 days and was 65% greater in TH when compared to NTH.
The total hospital charge on hospitalization was higher in TH at $101837(97566-106108) compared to $85422 for nonteaching. Post-procedure complications of Pancreatitis(OR: 0.87)and Hemorrhage(OR: 0.82) were lower in TH but increased in Bile Leak(OR: 2.03) and Infections(OR: 3.09) compared to NTH.
Discussion: Our study reveals that TH exhibits higher mortality rates, longer hospital stays, and greater costs for ERCP in biliary strictures, but they manage complications more effectively. Complications like pancreatitis and hemorrhage were lower in TH compared to NTH, aligning with prior studies highlighting the expertise of TH in handling complex cases. However, increased bile leaks and infections suggest areas for improvement. These findings align with existing literature emphasizing the dual-edged nature of care in teaching hospitals, where advanced expertise coexists with higher immediate risks and costs.
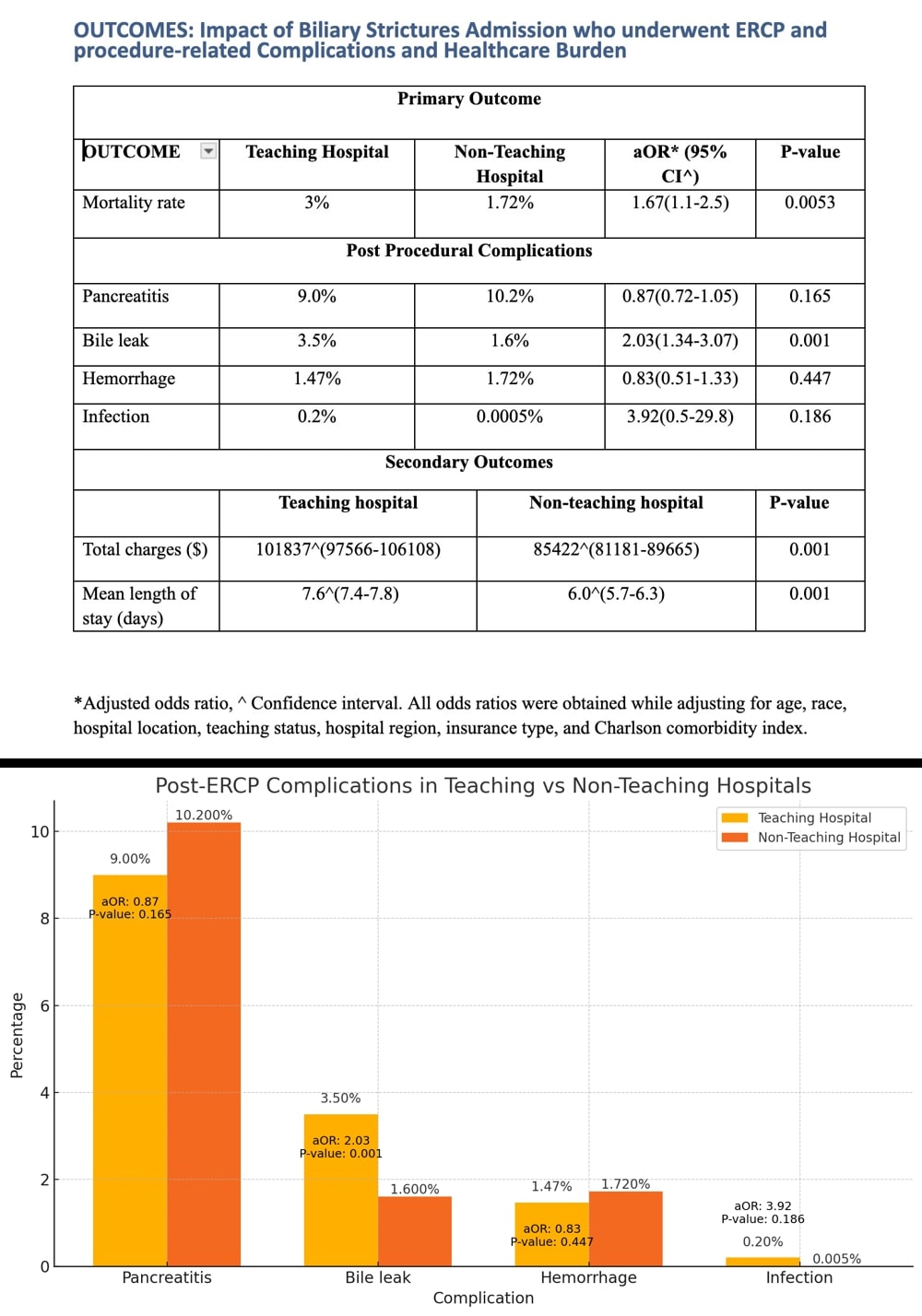
Figure: OUTCOMES: Impact of Biliary Strictures Admission who underwent ERCP and procedure-related Complications and Healthcare Burden
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Gautam Maddineni indicated no relevant financial relationships.
Akram Ahmad indicated no relevant financial relationships.
Zaid Ansari indicated no relevant financial relationships.
Tilak Shah indicated no relevant financial relationships.
Gautam Maddineni, MD1, Akram Ahmad, MBBS2, Zaid Ansari, MD3, Tilak Upendra. Shah, MD2. P3438 - Impact of Hospital Type on ERCP Outcomes for Biliary Strictures: A Comparative Analysis of Teaching vs Non-Teaching Hospitals (2016-2019), ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
