Tuesday Poster Session
Category: Biliary/Pancreas
P3446 - Pulmonary Embolism in Chronic Pancreatitis: A Retrospective Analysis of Predictors and Clinical Outcomes
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpg)
Raj H. Patel, MD
St. Mary Medical Center
Bensalem, PA
Presenting Author(s)
Raj H. Patel, MD1, Charmy Parikh, MD2, Sneh Sonaiya, MD3, Pratiksha Moliya, MD4, Yash R. Shah, MD5, Kartikeya Kaul, MD6, Aneri Parikh, MBBS7
1St. Mary Medical Center, Bensalem, PA; 2Mercy Catholic Medical Center, Darby, PA; 3University of Nevada, Las Vegas, NV; 4Jamaica Hospital Medical Center, Queens, NY; 5Trinity Health Oakland / Wayne State University School of Medicine, Pontiac, MI; 6St. Mary Medical Center, Langhorne, PA; 7Smt. NHL Municipal Medical College, Ahmedabad, Gujarat, India
Introduction: Chronic pancreatitis (CP) affects 5 to 12 out of every 100,000 adults and is characterized by a prolonged and complex clinical course. Pulmonary embolism (PE), though rare, is a serious complication in a large number of hospitalized patients. From previously published data, it can be hypothesized that CP which is a chronic inflammatory disorder can be one of the pro-thrombotic triggers contributing to the development of PE. We aim to identify the predictors of PE in patients with CP and analyze its impact on clinical outcomes to provide insights that could lead to targeted interventions to improve patient care.
Methods: A retrospective multivariate analysis was done to investigate predictors of PE in hospitalized chronic pancreatitis patients throughout the US. Our study utilized the National Inpatient Sample (NIS) database from 2016 to 2020, after propensity score matching. We also assessed secondary outcomes including mortality rate, length of hospital stay, and cost
of hospitalization.
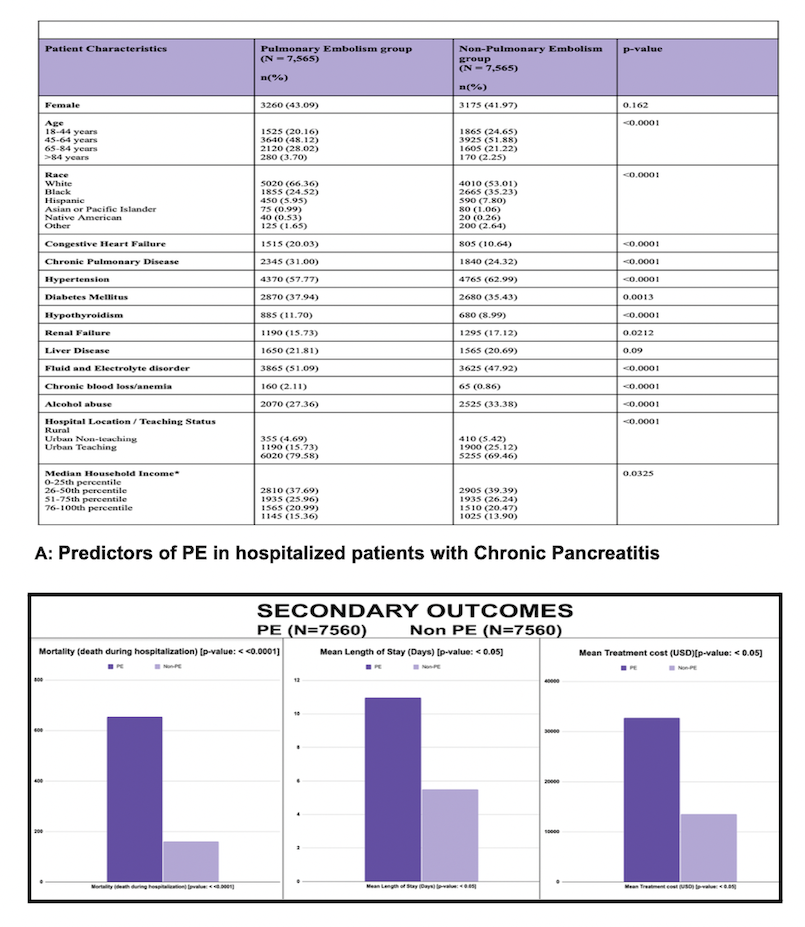
Results: 7565 CP patients with PE and 7565 CP patients without the development of PE were analyzed after propensity score matching. Significant predictors of PE in patients with CP include older age (OR: 1.52, 95% CI: 1.41-1.63, p< 0.0001), White race (OR: 1.75, 95% CI: 1.32-2.32, p< 0.0001), congestive heart failure (OR: 2.10, 95% CI: 1.45-3.05, p< 0.0001), chronic pulmonary
disease (OR: 1.40, 95% CI: 1.18-1.66, p< 0.0001), diabetes mellitus (OR: 1.11, 95% CI: 1.05-1.18, p< 0.05), fluid and electrolyte disorder (OR: 1.14, 95% CI: 1.05-1.18, p< 0.0001), chronic blood loss/anemia (OR: 2.49, 95% CI: 2.34-2.66, p< 0.0001), and treatment in urban teaching facilities (OR: 1.71, 95% CI: 1.54-1.89, p< 0.0001). PE in patients with CP was associated with significantly high all-cause mortality compared to the non-PE group (OR: 4.39, 95% CI: 2.97 to 6.51, p< 0.0001). PE in CP patients is also associated with a higher length of hospital stay and higher treatment cost compared to the non-PE group (10.97 days vs 5.51 days, p< 0.05; $32,747 vs $13,549, p< 0.05).
Discussion: This highlights the potential predictors of PE in CP patients including older age, White race, and comorbid conditions such as congestive heart failure and chronic pulmonary disease. PE in CP patients is associated with increased all-cause mortality, longer hospital stays, and higher treatment costs. This underscores the need for targeted intervention to manage PE in CP patients to improve patient outcomes and reduce healthcare costs.
Disclosures:
Raj H. Patel, MD1, Charmy Parikh, MD2, Sneh Sonaiya, MD3, Pratiksha Moliya, MD4, Yash R. Shah, MD5, Kartikeya Kaul, MD6, Aneri Parikh, MBBS7. P3446 - Pulmonary Embolism in Chronic Pancreatitis: A Retrospective Analysis of Predictors and Clinical Outcomes, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1St. Mary Medical Center, Bensalem, PA; 2Mercy Catholic Medical Center, Darby, PA; 3University of Nevada, Las Vegas, NV; 4Jamaica Hospital Medical Center, Queens, NY; 5Trinity Health Oakland / Wayne State University School of Medicine, Pontiac, MI; 6St. Mary Medical Center, Langhorne, PA; 7Smt. NHL Municipal Medical College, Ahmedabad, Gujarat, India
Introduction: Chronic pancreatitis (CP) affects 5 to 12 out of every 100,000 adults and is characterized by a prolonged and complex clinical course. Pulmonary embolism (PE), though rare, is a serious complication in a large number of hospitalized patients. From previously published data, it can be hypothesized that CP which is a chronic inflammatory disorder can be one of the pro-thrombotic triggers contributing to the development of PE. We aim to identify the predictors of PE in patients with CP and analyze its impact on clinical outcomes to provide insights that could lead to targeted interventions to improve patient care.
Methods: A retrospective multivariate analysis was done to investigate predictors of PE in hospitalized chronic pancreatitis patients throughout the US. Our study utilized the National Inpatient Sample (NIS) database from 2016 to 2020, after propensity score matching. We also assessed secondary outcomes including mortality rate, length of hospital stay, and cost
of hospitalization.
Results: 7565 CP patients with PE and 7565 CP patients without the development of PE were analyzed after propensity score matching. Significant predictors of PE in patients with CP include older age (OR: 1.52, 95% CI: 1.41-1.63, p< 0.0001), White race (OR: 1.75, 95% CI: 1.32-2.32, p< 0.0001), congestive heart failure (OR: 2.10, 95% CI: 1.45-3.05, p< 0.0001), chronic pulmonary
disease (OR: 1.40, 95% CI: 1.18-1.66, p< 0.0001), diabetes mellitus (OR: 1.11, 95% CI: 1.05-1.18, p< 0.05), fluid and electrolyte disorder (OR: 1.14, 95% CI: 1.05-1.18, p< 0.0001), chronic blood loss/anemia (OR: 2.49, 95% CI: 2.34-2.66, p< 0.0001), and treatment in urban teaching facilities (OR: 1.71, 95% CI: 1.54-1.89, p< 0.0001). PE in patients with CP was associated with significantly high all-cause mortality compared to the non-PE group (OR: 4.39, 95% CI: 2.97 to 6.51, p< 0.0001). PE in CP patients is also associated with a higher length of hospital stay and higher treatment cost compared to the non-PE group (10.97 days vs 5.51 days, p< 0.05; $32,747 vs $13,549, p< 0.05).
Discussion: This highlights the potential predictors of PE in CP patients including older age, White race, and comorbid conditions such as congestive heart failure and chronic pulmonary disease. PE in CP patients is associated with increased all-cause mortality, longer hospital stays, and higher treatment costs. This underscores the need for targeted intervention to manage PE in CP patients to improve patient outcomes and reduce healthcare costs.
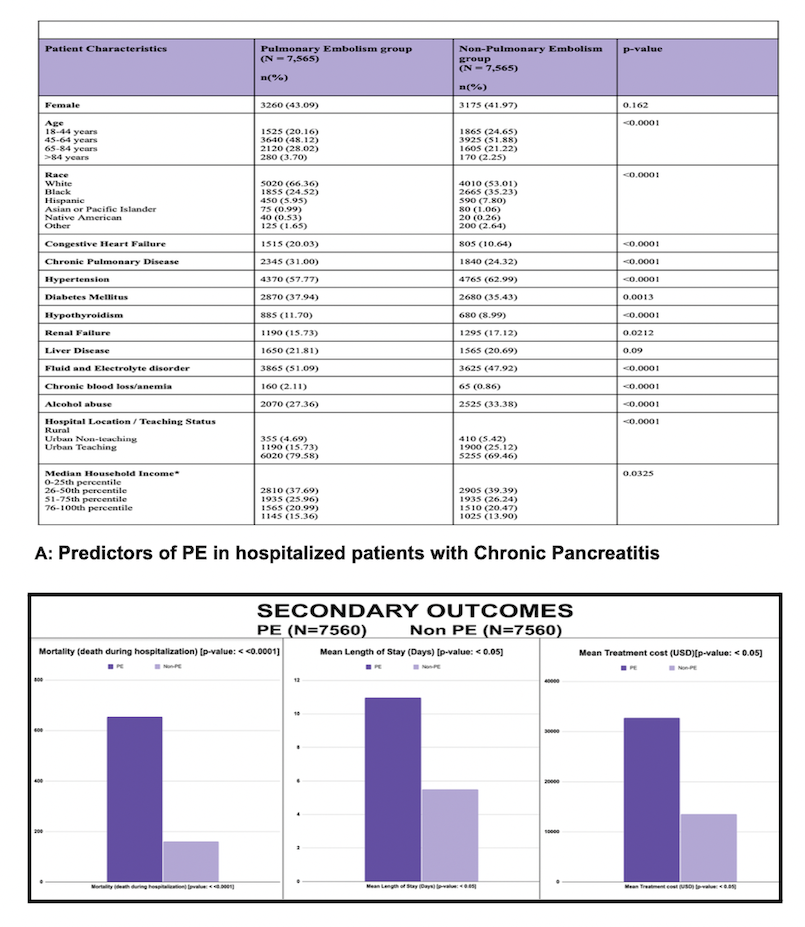
Figure: Predictors of Pulmonary Embolism in Hospitalized Chronic Pancreatitis Patients with Secondary Outcomes
Disclosures:
Raj Patel indicated no relevant financial relationships.
Charmy Parikh indicated no relevant financial relationships.
Sneh Sonaiya indicated no relevant financial relationships.
Pratiksha Moliya indicated no relevant financial relationships.
Yash Shah indicated no relevant financial relationships.
Kartikeya Kaul indicated no relevant financial relationships.
Aneri Parikh indicated no relevant financial relationships.
Raj H. Patel, MD1, Charmy Parikh, MD2, Sneh Sonaiya, MD3, Pratiksha Moliya, MD4, Yash R. Shah, MD5, Kartikeya Kaul, MD6, Aneri Parikh, MBBS7. P3446 - Pulmonary Embolism in Chronic Pancreatitis: A Retrospective Analysis of Predictors and Clinical Outcomes, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
