Tuesday Poster Session
Category: Biliary/Pancreas
P3453 - Impact of Glucagon-Like Peptide-1 Receptor Agonist on Gallbladder and Biliary Diseases
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Khaled Alsabbagh Alchirazi, MD
Aurora Healthcare
Brookfield, WI
Presenting Author(s)
Khaled Alsabbagh Alchirazi, MD1, Michelle Baliss, DO2, Ahmed El Telbany, MD, MPH3, Muaz Alsabbagh, MD4, Saqr Alsakarneh, MD5, Wissam Kiwan, MD6, Mohammad Bilal, MD7
1Aurora Healthcare, Brookfield, WI; 2SSM Health Saint Louis University Hospital, St. Louis, MO; 3University of New Mexico, Albuquerque, NM; 4Cleveland Clinic, Cleveland, OH; 5University of Missouri - Kansas City School of Medicine, Kansas City, MO; 6Saint Louis University, St. Louis, MO; 7University of Minnesota and Minneapolis VA Health Care System, Minneapolis, MN
Introduction: Glucagon-like peptide-1 receptor agonists (GLP-1 RAs) are commonly prescribed for managing type 2 diabetes (T2DM) and obesity due to their benefits in controlling blood sugar levels and reducing weight. Previous studies have suggested an increased risk of gallbladder disorders among patients treated with GLP-1 RAs compared to those on placebo due to their potential role in inhibiting the gallbladder motility and delaying gallbladder emptying, but data are controversial. This study aims to investigate the association between the use of GLP-1 RAs and biliary diseases, offering new insights due to the limited research in this area.
Methods: We conducted a retrospective cohort study using data from the TriNetX database, covering the period 2018- 2023. Our research focused on patients with T2DM, comparing those who were treated with GLP-1 RAs to those not receiving these medications. To control for potential confounding factors, we matched the cohorts based on age, gender, race, ethnicity, and pre-existing health conditions. The primary outcome was the risk of biliary diseases within 6 months and 1 year from GLP-1 RAs prescription. Statistical analysis was performed using adjusted hazard ratios (HR) with 95% confidence intervals (CI), to assess the impact of GLP-1 RAs on biliary complications.
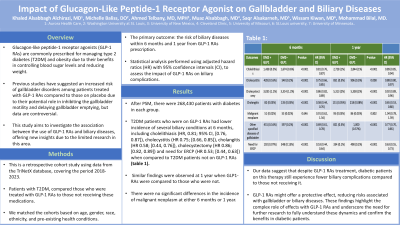
Results: After propensity score matching, there were 268,430 patients with diabetes in each group. T2DM patients who were on GLP-1 RAs had lower incidence of several biliary conditions at 6 months, including cholelithiasis (HR, 0.81; 95% CI, [0.76, 0.87]), cholecystitis (HR 0.75; [0.66, 0.85]), cholangitis (HR 0.58; [0.44, 0.76]),cholecystectomy (HR 0.86; [0.82, 0.89]) and need for ERCP (HR 0.53; [0.44, 0.63]) when compared to T2DM patients not on GLP-1 RAs (table 1). Similar findings were observed at 1 year when GLP1-RAs were compared to those who were not. However, there were no significant differences in the incidence of malignant neoplasm at either 6 months or 1 year.
Discussion: Using large scale retrospective database, our data suggest that despite GLP-1 RAs treatment, diabetic patients on this therapy still experience fewer biliary complications compared to those not receiving it. This indicates that GLP-1 RAs might offer a protective effect, reducing risks associated with gallbladder or biliary diseases. These findings highlight the complex role of effects with GLP-1 RAs and underscore the need for further research to fully understand these dynamics and confirm the benefits in diabetic patients.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Khaled Alsabbagh Alchirazi, MD1, Michelle Baliss, DO2, Ahmed El Telbany, MD, MPH3, Muaz Alsabbagh, MD4, Saqr Alsakarneh, MD5, Wissam Kiwan, MD6, Mohammad Bilal, MD7. P3453 - Impact of Glucagon-Like Peptide-1 Receptor Agonist on Gallbladder and Biliary Diseases, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Aurora Healthcare, Brookfield, WI; 2SSM Health Saint Louis University Hospital, St. Louis, MO; 3University of New Mexico, Albuquerque, NM; 4Cleveland Clinic, Cleveland, OH; 5University of Missouri - Kansas City School of Medicine, Kansas City, MO; 6Saint Louis University, St. Louis, MO; 7University of Minnesota and Minneapolis VA Health Care System, Minneapolis, MN
Introduction: Glucagon-like peptide-1 receptor agonists (GLP-1 RAs) are commonly prescribed for managing type 2 diabetes (T2DM) and obesity due to their benefits in controlling blood sugar levels and reducing weight. Previous studies have suggested an increased risk of gallbladder disorders among patients treated with GLP-1 RAs compared to those on placebo due to their potential role in inhibiting the gallbladder motility and delaying gallbladder emptying, but data are controversial. This study aims to investigate the association between the use of GLP-1 RAs and biliary diseases, offering new insights due to the limited research in this area.
Methods: We conducted a retrospective cohort study using data from the TriNetX database, covering the period 2018- 2023. Our research focused on patients with T2DM, comparing those who were treated with GLP-1 RAs to those not receiving these medications. To control for potential confounding factors, we matched the cohorts based on age, gender, race, ethnicity, and pre-existing health conditions. The primary outcome was the risk of biliary diseases within 6 months and 1 year from GLP-1 RAs prescription. Statistical analysis was performed using adjusted hazard ratios (HR) with 95% confidence intervals (CI), to assess the impact of GLP-1 RAs on biliary complications.
Results: After propensity score matching, there were 268,430 patients with diabetes in each group. T2DM patients who were on GLP-1 RAs had lower incidence of several biliary conditions at 6 months, including cholelithiasis (HR, 0.81; 95% CI, [0.76, 0.87]), cholecystitis (HR 0.75; [0.66, 0.85]), cholangitis (HR 0.58; [0.44, 0.76]),cholecystectomy (HR 0.86; [0.82, 0.89]) and need for ERCP (HR 0.53; [0.44, 0.63]) when compared to T2DM patients not on GLP-1 RAs (table 1). Similar findings were observed at 1 year when GLP1-RAs were compared to those who were not. However, there were no significant differences in the incidence of malignant neoplasm at either 6 months or 1 year.
Discussion: Using large scale retrospective database, our data suggest that despite GLP-1 RAs treatment, diabetic patients on this therapy still experience fewer biliary complications compared to those not receiving it. This indicates that GLP-1 RAs might offer a protective effect, reducing risks associated with gallbladder or biliary diseases. These findings highlight the complex role of effects with GLP-1 RAs and underscore the need for further research to fully understand these dynamics and confirm the benefits in diabetic patients.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Khaled Alsabbagh Alchirazi indicated no relevant financial relationships.
Michelle Baliss indicated no relevant financial relationships.
Ahmed El Telbany indicated no relevant financial relationships.
Muaz Alsabbagh indicated no relevant financial relationships.
Saqr Alsakarneh indicated no relevant financial relationships.
Wissam Kiwan indicated no relevant financial relationships.
Mohammad Bilal: Boston Scientific – Consultant. Cook endoscopy – Speakers Bureau.
Khaled Alsabbagh Alchirazi, MD1, Michelle Baliss, DO2, Ahmed El Telbany, MD, MPH3, Muaz Alsabbagh, MD4, Saqr Alsakarneh, MD5, Wissam Kiwan, MD6, Mohammad Bilal, MD7. P3453 - Impact of Glucagon-Like Peptide-1 Receptor Agonist on Gallbladder and Biliary Diseases, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
