Tuesday Poster Session
Category: Biliary/Pancreas
P3462 - Patients Managed for Chronic Pancreatitis in a VA Population Are Done So With Low Diagnostic Confidence
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Claire Beamish, MD
Dartmouth Hitchcock Medical Center
Lebanon, NH
Presenting Author(s)
Claire Beamish, MD, Jonathan Beard, MD, Sharon M. Thomson, MD, David Klibansky, MD
Dartmouth Hitchcock Medical Center, Lebanon, NH
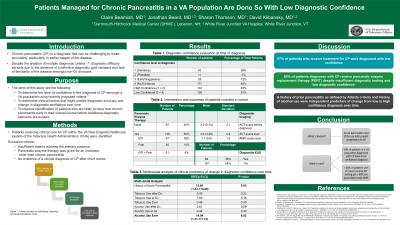
Introduction: Chronic pancreatitis (CP) is a progressive chronic inflammatory condition resulting in irreversible anatomic and functional changes in the pancreas. Although multiple diagnostic frameworks exist for chronic pancreatitis, there is no definitive gold standards. The aim of this study is to determine the level of confidence in the diagnosis of CP and to identify clinical factors that might predict a change in diagnostic confidence over time.
Methods: A retrospective chart review was performed for patients receiving clinical care for CP within the Veterans Health Administration New England Healthcare System. Exclusion criteria included the following: insufficient data to address the primary outcome; pancreatic enzyme replacement therapy (PERT) was given for an indication other than CP; chart review demonstrated no evidence of a clinical diagnosis of CP. A total of 245 patients were included in the study and a diagnostic confidence-level was assigned based on clinical features and imaging criteria. The primary outcome of the study was a determination of the diagnostic confidence level in patients being treated for CP at initial diagnosis.
Results: At the time of CP diagnosis, 139 patients (57%) had little to no evidence supporting this diagnosis. Statistical analysis was subsequently completed to understand which variables predicted progression from a low-confidence to a high-confidence diagnosis. Amongst the 139 patients with a low-confidence score at the time of diagnosis, 17% of patients had a change in diagnostic score from low to high-confidence over 1508.6 patient-years of follow up. On multivariate analysis, moderate alcohol use (OR 14, CI 1.3 – 111) and acute pancreatitis (OR 12.8, CI 1.4 – 113.7) were independently predictive for progression from low to high-confidence diagnosis.
Discussion: Applying clinical criteria and imaging findings, 57% of the patients in this VA population were receiving care for CP with low confidence in that diagnosis, which is much higher than prior comparable studies that demonstrated ~15% low-confidence diagnoses. This has multiple health consequences, including medical error and excess cost. For example, 60% of the patients in our study population were treated with costly PERT for CP but less than 20% had objective testing for exocrine pancreatic insufficiency. This study ultimately underscores the importance of refining and clearly delineating diagnostic strategies for CP, particularly within the Veteran’s Health Administration.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Claire Beamish, MD, Jonathan Beard, MD, Sharon M. Thomson, MD, David Klibansky, MD. P3462 - Patients Managed for Chronic Pancreatitis in a VA Population Are Done So With Low Diagnostic Confidence, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Dartmouth Hitchcock Medical Center, Lebanon, NH
Introduction: Chronic pancreatitis (CP) is a progressive chronic inflammatory condition resulting in irreversible anatomic and functional changes in the pancreas. Although multiple diagnostic frameworks exist for chronic pancreatitis, there is no definitive gold standards. The aim of this study is to determine the level of confidence in the diagnosis of CP and to identify clinical factors that might predict a change in diagnostic confidence over time.
Methods: A retrospective chart review was performed for patients receiving clinical care for CP within the Veterans Health Administration New England Healthcare System. Exclusion criteria included the following: insufficient data to address the primary outcome; pancreatic enzyme replacement therapy (PERT) was given for an indication other than CP; chart review demonstrated no evidence of a clinical diagnosis of CP. A total of 245 patients were included in the study and a diagnostic confidence-level was assigned based on clinical features and imaging criteria. The primary outcome of the study was a determination of the diagnostic confidence level in patients being treated for CP at initial diagnosis.
Results: At the time of CP diagnosis, 139 patients (57%) had little to no evidence supporting this diagnosis. Statistical analysis was subsequently completed to understand which variables predicted progression from a low-confidence to a high-confidence diagnosis. Amongst the 139 patients with a low-confidence score at the time of diagnosis, 17% of patients had a change in diagnostic score from low to high-confidence over 1508.6 patient-years of follow up. On multivariate analysis, moderate alcohol use (OR 14, CI 1.3 – 111) and acute pancreatitis (OR 12.8, CI 1.4 – 113.7) were independently predictive for progression from low to high-confidence diagnosis.
Discussion: Applying clinical criteria and imaging findings, 57% of the patients in this VA population were receiving care for CP with low confidence in that diagnosis, which is much higher than prior comparable studies that demonstrated ~15% low-confidence diagnoses. This has multiple health consequences, including medical error and excess cost. For example, 60% of the patients in our study population were treated with costly PERT for CP but less than 20% had objective testing for exocrine pancreatic insufficiency. This study ultimately underscores the importance of refining and clearly delineating diagnostic strategies for CP, particularly within the Veteran’s Health Administration.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Claire Beamish indicated no relevant financial relationships.
Jonathan Beard: Phathom Pharmaceuticals – Stock-publicly held company(excluding mutual/index funds).
Sharon Thomson indicated no relevant financial relationships.
David Klibansky indicated no relevant financial relationships.
Claire Beamish, MD, Jonathan Beard, MD, Sharon M. Thomson, MD, David Klibansky, MD. P3462 - Patients Managed for Chronic Pancreatitis in a VA Population Are Done So With Low Diagnostic Confidence, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

