Tuesday Poster Session
Category: Biliary/Pancreas
P3479 - Differences In Clinical Outcomes Between Acute Pancreatitis Caucasian, African American, and Asian Population With Metabolic Dysfunction-Associated Steatotic Liver Disease
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

M Kenan Rahima, MD
TriHealth Good Samaritan Hospital
Cincinnati, OH
Presenting Author(s)
M Kenan Rahima, MD1, Mohamad Hijazi, MD1, Mhd Kutaiba Albuni, MD2, Bassel Bitar, MD1, Tarek Aboursheid, MD3, Fernando R. Mateo, MD4, Venkata Muddana, MD4
1TriHealth Good Samaritan Hospital, Cincinnati, OH; 2TriHealth, Doha, Ad Dawhah, Qatar; 3Ascension Saint Francis Hospital, Evanston, IL; 4TriHealth, Cincinnati, OH
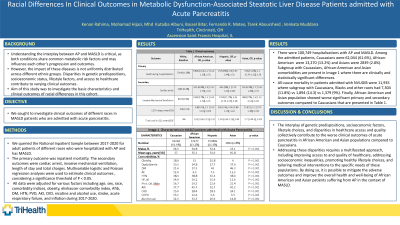
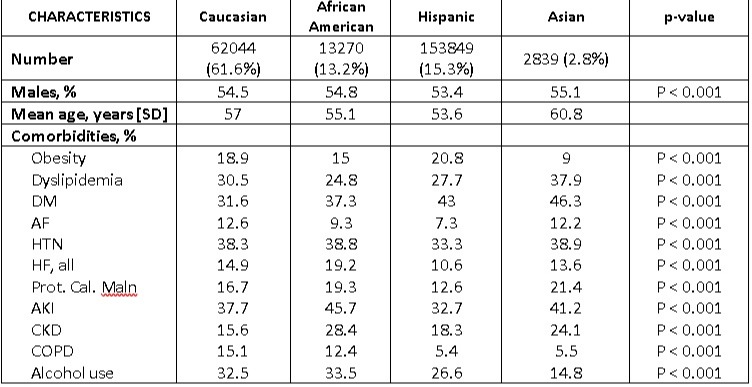
Introduction: Understanding the interplay between AP and MASLD is critical, as both conditions share common metabolic risk factors and may influence each other’s progression and outcomes. However, the impact of these diseases is not uniformly distributed across different ethnic groups. This study aimed to investigate the basic characteristics and clinical outcomes of racial differences in this cohort.
Methods: We queried the National Inpatient Sample between 2017 and 2020 for adult patients of different races who were hospitalized with AP and had MASLD. The primary outcome was inpatient mortality. The secondary outcomes were cardiac arrest, invasive mechanical ventilation, length of stay (LOS), and total hospital cost. Multivariable logistic and Poisson regression analyses were used to estimate clinical outcomes, considering a significance threshold of P < 0.05. All data were adjusted for various factors including age, sex, race, obesity, elixhauser comorbidity index, Afib, DM, HTN, PVD, AKI, CKD, alcohol use, stroke, acute respiratory failure, and inflation during 2017-2020.
Results: There were 100,749 hospitalizations with AP and MASLD. Among the admitted patients, Caucasians were 62,044 (61.6%), African-Americans were 13,270 (13.2%) and Asians were 2839 (2.8%). Subgroups with Caucasian, African-American, and Asian comorbidities are present in Image 1 where there are clinically and statistically significant differences. All-cause mortality in patients admitted with NVUGIB was 11,935 whereas the subgroup with Caucasians, Blacks, and Asian population had 7,304 (11.8%) vs 1,894 (14.3) vs 1,379 (9%). Finally, African-American and Asian populations showed worse significant primary and secondary outcomes compared to Caucasians which are presented in Table 1.
Discussion: The interplay of genetic predispositions, socioeconomic factors, lifestyle choices, and disparities in healthcare access and quality collectively contribute to the worse clinical outcomes of acute pancreatitis in African American and Asian populations compared to Caucasians. Addressing these disparities requires a multifaceted approach, including improving access to and quality of healthcare, addressing socioeconomic inequalities, promoting healthy lifestyle choices, and tailoring medical interventions to the specific needs of these populations. By doing so, it is possible to mitigate the adverse outcomes and improve the overall health and well-being of African American and Asian patients suffering from AP in the context of MASLD.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
M Kenan Rahima, MD1, Mohamad Hijazi, MD1, Mhd Kutaiba Albuni, MD2, Bassel Bitar, MD1, Tarek Aboursheid, MD3, Fernando R. Mateo, MD4, Venkata Muddana, MD4. P3479 - Differences In Clinical Outcomes Between Acute Pancreatitis Caucasian, African American, and Asian Population With Metabolic Dysfunction-Associated Steatotic Liver Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1TriHealth Good Samaritan Hospital, Cincinnati, OH; 2TriHealth, Doha, Ad Dawhah, Qatar; 3Ascension Saint Francis Hospital, Evanston, IL; 4TriHealth, Cincinnati, OH
Introduction: Understanding the interplay between AP and MASLD is critical, as both conditions share common metabolic risk factors and may influence each other’s progression and outcomes. However, the impact of these diseases is not uniformly distributed across different ethnic groups. This study aimed to investigate the basic characteristics and clinical outcomes of racial differences in this cohort.
Methods: We queried the National Inpatient Sample between 2017 and 2020 for adult patients of different races who were hospitalized with AP and had MASLD. The primary outcome was inpatient mortality. The secondary outcomes were cardiac arrest, invasive mechanical ventilation, length of stay (LOS), and total hospital cost. Multivariable logistic and Poisson regression analyses were used to estimate clinical outcomes, considering a significance threshold of P < 0.05. All data were adjusted for various factors including age, sex, race, obesity, elixhauser comorbidity index, Afib, DM, HTN, PVD, AKI, CKD, alcohol use, stroke, acute respiratory failure, and inflation during 2017-2020.
Results: There were 100,749 hospitalizations with AP and MASLD. Among the admitted patients, Caucasians were 62,044 (61.6%), African-Americans were 13,270 (13.2%) and Asians were 2839 (2.8%). Subgroups with Caucasian, African-American, and Asian comorbidities are present in Image 1 where there are clinically and statistically significant differences. All-cause mortality in patients admitted with NVUGIB was 11,935 whereas the subgroup with Caucasians, Blacks, and Asian population had 7,304 (11.8%) vs 1,894 (14.3) vs 1,379 (9%). Finally, African-American and Asian populations showed worse significant primary and secondary outcomes compared to Caucasians which are presented in Table 1.
Discussion: The interplay of genetic predispositions, socioeconomic factors, lifestyle choices, and disparities in healthcare access and quality collectively contribute to the worse clinical outcomes of acute pancreatitis in African American and Asian populations compared to Caucasians. Addressing these disparities requires a multifaceted approach, including improving access to and quality of healthcare, addressing socioeconomic inequalities, promoting healthy lifestyle choices, and tailoring medical interventions to the specific needs of these populations. By doing so, it is possible to mitigate the adverse outcomes and improve the overall health and well-being of African American and Asian patients suffering from AP in the context of MASLD.
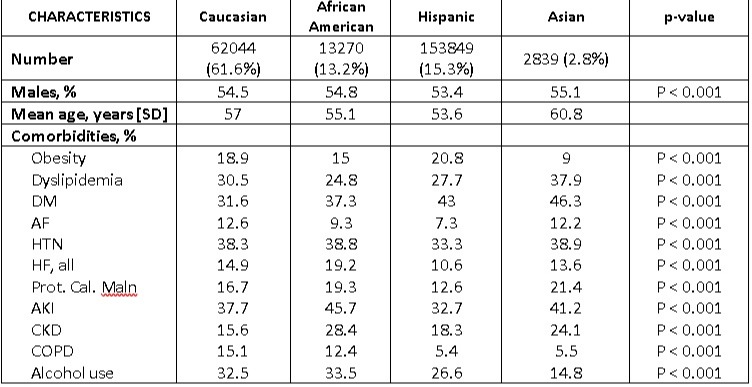
Figure: Image 1
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
M Kenan Rahima indicated no relevant financial relationships.
Mohamad Hijazi indicated no relevant financial relationships.
Mhd Kutaiba Albuni indicated no relevant financial relationships.
Bassel Bitar indicated no relevant financial relationships.
Tarek Aboursheid indicated no relevant financial relationships.
Fernando Mateo indicated no relevant financial relationships.
Venkata Muddana indicated no relevant financial relationships.
M Kenan Rahima, MD1, Mohamad Hijazi, MD1, Mhd Kutaiba Albuni, MD2, Bassel Bitar, MD1, Tarek Aboursheid, MD3, Fernando R. Mateo, MD4, Venkata Muddana, MD4. P3479 - Differences In Clinical Outcomes Between Acute Pancreatitis Caucasian, African American, and Asian Population With Metabolic Dysfunction-Associated Steatotic Liver Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
