Tuesday Poster Session
Category: Biliary/Pancreas
P3490 - Characterizing Individuals With Recurrent Acute Pancreatitis and Exocrine Pancreatic Insufficiency: Findings From the PACT-CP Registry
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- JD
Jane A. Diamond, MS, FNP
Mayo Clinic
Jacksonville, FL
Presenting Author(s)
Jane A.. Diamond, MS, FNP1, Patrick S.. Yachimski, MD, MPH2, Samer Al-Kaade, MD3, Janine Twal, PharmD4, Jennifer Pack, MSN4, Yasmin Hernandez-Barco, MD5
1Mayo Clinic, Jacksonville, FL; 2Vanderbilt University Medical Center, Nashville, TN; 3Mercy Clinic Gastroenterology, St. Louis, MO; 4Nestlé Health Science, Bridgewater, NJ; 5Massachusetts General Hospital, Boston, MA
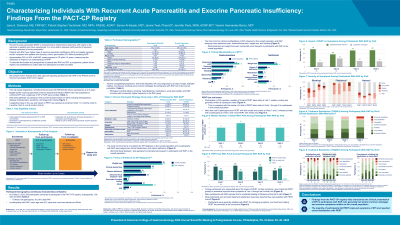
Introduction: Patients with recurrent acute pancreatitis (RAP) have higher rates of exocrine pancreatic insufficiency (EPI), greater symptom burden, and higher rates of healthcare utilization compared with patients who develop chronic pancreatitis (CP) without preceding RAP. About 25–50% of all RAP cases progress to CP within 10 years, underscoring the imperative to improve our understanding of RAP. To describe the burden and perspectives of patients with RAP and EPI, a prospective, patient-driven registry was established to collect data from participants and their providers. We present interim findings from data captured regarding participants with RAP in the PAtient-CenTric Chronic Pancreatitis (PACT-CP) registry.
Methods: This US-based longitudinal, noninterventional study (NCT05762445) follows participants up to 5 years. Adults diagnosed with RAP or CP at enrollment, who were receiving pancreatic enzyme replacement therapy (PERT), and had suspected/confirmed EPI by a healthcare practitioner were enrolled in the registry. Data were gathered via participant and provider questionnaires on items including demographics, disease characteristics, symptoms, and diagnostic criteria.
Results: As of May 5, 2024, there were 200 participants enrolled in the PACT-CP registry; of these 200 participants, 30 had RAP. Mean age was 55.2 years, most participants with RAP were female (59.3%) and White (92.6%) (Table). Alcohol susceptibility/progression (36.7%), late onset idiopathic CP (occurring beyond 35 years of age; 30.0%), and tobacco smoking (26.7%) were common etiologies for participants with RAP. The most common forms of evidence for EPI diagnosis were weight loss (56.7%), clinical steatorrhea (40.0%), and vitamin deficiency (26.7%). The most common clinical manifestations of EPI observed in this population were abdominal pain (90.0%), diarrhea/loose stool (70.0%), weight loss (63.3%), and bloating (56.7%). Participants (n=24) reported a median of 6 pills of PERT taken daily at Visit 1; median number was generally similar at subsequent visits. Most participants responding about PERT impact on symptoms at Visit 1 through the 9-month (mo) visit noted PERT greatly/somewhat improved symptoms (Visit 1, 79.1% [N=24]; 3-mo, 56.3% [N=16]; 6-mo, 73.7% [N=19]; 9-mo, 75.0% [N=12]).
Discussion: Findings from the PACT-CP registry help characterize the clinical presentation of EPI in participants with RAP. The majority of participants felt PERT improved symptoms of EPI.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Jane A.. Diamond, MS, FNP1, Patrick S.. Yachimski, MD, MPH2, Samer Al-Kaade, MD3, Janine Twal, PharmD4, Jennifer Pack, MSN4, Yasmin Hernandez-Barco, MD5. P3490 - Characterizing Individuals With Recurrent Acute Pancreatitis and Exocrine Pancreatic Insufficiency: Findings From the PACT-CP Registry, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Mayo Clinic, Jacksonville, FL; 2Vanderbilt University Medical Center, Nashville, TN; 3Mercy Clinic Gastroenterology, St. Louis, MO; 4Nestlé Health Science, Bridgewater, NJ; 5Massachusetts General Hospital, Boston, MA
Introduction: Patients with recurrent acute pancreatitis (RAP) have higher rates of exocrine pancreatic insufficiency (EPI), greater symptom burden, and higher rates of healthcare utilization compared with patients who develop chronic pancreatitis (CP) without preceding RAP. About 25–50% of all RAP cases progress to CP within 10 years, underscoring the imperative to improve our understanding of RAP. To describe the burden and perspectives of patients with RAP and EPI, a prospective, patient-driven registry was established to collect data from participants and their providers. We present interim findings from data captured regarding participants with RAP in the PAtient-CenTric Chronic Pancreatitis (PACT-CP) registry.
Methods: This US-based longitudinal, noninterventional study (NCT05762445) follows participants up to 5 years. Adults diagnosed with RAP or CP at enrollment, who were receiving pancreatic enzyme replacement therapy (PERT), and had suspected/confirmed EPI by a healthcare practitioner were enrolled in the registry. Data were gathered via participant and provider questionnaires on items including demographics, disease characteristics, symptoms, and diagnostic criteria.
Results: As of May 5, 2024, there were 200 participants enrolled in the PACT-CP registry; of these 200 participants, 30 had RAP. Mean age was 55.2 years, most participants with RAP were female (59.3%) and White (92.6%) (Table). Alcohol susceptibility/progression (36.7%), late onset idiopathic CP (occurring beyond 35 years of age; 30.0%), and tobacco smoking (26.7%) were common etiologies for participants with RAP. The most common forms of evidence for EPI diagnosis were weight loss (56.7%), clinical steatorrhea (40.0%), and vitamin deficiency (26.7%). The most common clinical manifestations of EPI observed in this population were abdominal pain (90.0%), diarrhea/loose stool (70.0%), weight loss (63.3%), and bloating (56.7%). Participants (n=24) reported a median of 6 pills of PERT taken daily at Visit 1; median number was generally similar at subsequent visits. Most participants responding about PERT impact on symptoms at Visit 1 through the 9-month (mo) visit noted PERT greatly/somewhat improved symptoms (Visit 1, 79.1% [N=24]; 3-mo, 56.3% [N=16]; 6-mo, 73.7% [N=19]; 9-mo, 75.0% [N=12]).
Discussion: Findings from the PACT-CP registry help characterize the clinical presentation of EPI in participants with RAP. The majority of participants felt PERT improved symptoms of EPI.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Jane Diamond indicated no relevant financial relationships.
Patrick Yachimski indicated no relevant financial relationships.
Samer Al-Kaade: Abbvie – Speakers Bureau. InterPace – Speakers Bureau.
Janine Twal: Nestle Health Science – Employee, Stock-publicly held company(excluding mutual/index funds).
Jennifer Pack: Nestlé Health Science – Employee.
Yasmin Hernandez-Barco: Amgen – Advisor or Review Panel Member. Nestlé health science – Advisor or Review Panel Member.
Jane A.. Diamond, MS, FNP1, Patrick S.. Yachimski, MD, MPH2, Samer Al-Kaade, MD3, Janine Twal, PharmD4, Jennifer Pack, MSN4, Yasmin Hernandez-Barco, MD5. P3490 - Characterizing Individuals With Recurrent Acute Pancreatitis and Exocrine Pancreatic Insufficiency: Findings From the PACT-CP Registry, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
