Tuesday Poster Session
Category: Biliary/Pancreas
P3495 - Association of Marijuana Use and the Severity of Idiopathic Acute Pancreatitis
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E

Suhail Sidhu, MD
CHI Health Creighton University Medical Center
Anaheim, CA
Presenting Author(s)
Suhail Sidhu, MD1, Walter Crum, MD2, Omar Alaber, MD2, Rahul Thusay, MA2, Nikhil Furtado, BS2, Ryan Walters, PhD2, Sandeep Mukherjee, MD2
1CHI Health Creighton University Medical Center, Fremont, CA; 2CHI Health Creighton University Medical Center, Omaha, NE
Introduction: Marijuana (MJ) is the most widely used illicit drug in the USA with an estimated lifetime prevalence of 44%. A systematic review of 26 studies with idiopathic pancreatitis and cannabis use reported that a majority of patients acknowledged an increase in MJ use prior to onset of acute pancreatitis. However, due to the small sample size, no definitive association could be made. With the increased recreational use of MJ, especially in light of the department of justice’s proposal to reschedule MJ as a schedule III substance, there may be an increased risk for the development of acute pancreatitis. Our goal is to build on these preliminary studies by reviewing the electronic medical records at CHI Hospitals between the 2017 - 2023 to determine if cannabis use is associated with the severity of acute idiopathic pancreatitis. Additionally, our goal was to analyze how physical, psychological, and socioeconomic hardships may impact the severity of pancreatitis.
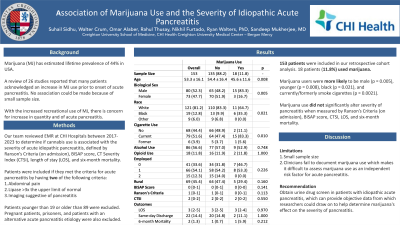
Methods: Severity of pancreatitis was defined by Ranson’s Criteria (on admission), BISAP score, CT Severity Index (CTSI), length of stay (LOS), and six-month mortality. Patients were included if they met the criteria for acute pancreatitis by having two of the following criteria: abdominal pain, lipase >3x the upper limit of normal, or imaging suggestive of pancreatitis. Patients younger than 19 or older than 89 were excluded. Pregnant patients, prisoners, and patients with an alternative acute pancreatitis etiology were also excluded.
Results: 153 patients were included in our retrospective cohort analysis. 18 patients (11.8%) used marijuana. In our cohort, Marijuana users were more likely to be male (p = 0.005), younger (p = 0.008), black (p = 0.021), and currently/formerly smoke cigarettes (p = 0.0021). Marijuana use did not statistically significantly alter severity of pancreatitis when measured by Ranson’s Criteria (on admission), BISAP score, CTSI, LOS, and six-month mortality.
Discussion: Beyond small sample size, one limitation of our study is that clinicians often fail to adequately detail a patient’s history with marijuana in the context of duration, frequency, and method of use. Therefore, it is difficult to assess marijuana use as an independent risk factor for acute pancreatitis. Recommending urine drug screens to patients with idiopathic acute pancreatitis may provide objective data from which researchers could draw on to determine mairjuana’s effect on the development/severity of acute pancreatitis.
Disclosures:
Suhail Sidhu, MD1, Walter Crum, MD2, Omar Alaber, MD2, Rahul Thusay, MA2, Nikhil Furtado, BS2, Ryan Walters, PhD2, Sandeep Mukherjee, MD2. P3495 - Association of Marijuana Use and the Severity of Idiopathic Acute Pancreatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1CHI Health Creighton University Medical Center, Fremont, CA; 2CHI Health Creighton University Medical Center, Omaha, NE
Introduction: Marijuana (MJ) is the most widely used illicit drug in the USA with an estimated lifetime prevalence of 44%. A systematic review of 26 studies with idiopathic pancreatitis and cannabis use reported that a majority of patients acknowledged an increase in MJ use prior to onset of acute pancreatitis. However, due to the small sample size, no definitive association could be made. With the increased recreational use of MJ, especially in light of the department of justice’s proposal to reschedule MJ as a schedule III substance, there may be an increased risk for the development of acute pancreatitis. Our goal is to build on these preliminary studies by reviewing the electronic medical records at CHI Hospitals between the 2017 - 2023 to determine if cannabis use is associated with the severity of acute idiopathic pancreatitis. Additionally, our goal was to analyze how physical, psychological, and socioeconomic hardships may impact the severity of pancreatitis.
Methods: Severity of pancreatitis was defined by Ranson’s Criteria (on admission), BISAP score, CT Severity Index (CTSI), length of stay (LOS), and six-month mortality. Patients were included if they met the criteria for acute pancreatitis by having two of the following criteria: abdominal pain, lipase >3x the upper limit of normal, or imaging suggestive of pancreatitis. Patients younger than 19 or older than 89 were excluded. Pregnant patients, prisoners, and patients with an alternative acute pancreatitis etiology were also excluded.
Results: 153 patients were included in our retrospective cohort analysis. 18 patients (11.8%) used marijuana. In our cohort, Marijuana users were more likely to be male (p = 0.005), younger (p = 0.008), black (p = 0.021), and currently/formerly smoke cigarettes (p = 0.0021). Marijuana use did not statistically significantly alter severity of pancreatitis when measured by Ranson’s Criteria (on admission), BISAP score, CTSI, LOS, and six-month mortality.
Discussion: Beyond small sample size, one limitation of our study is that clinicians often fail to adequately detail a patient’s history with marijuana in the context of duration, frequency, and method of use. Therefore, it is difficult to assess marijuana use as an independent risk factor for acute pancreatitis. Recommending urine drug screens to patients with idiopathic acute pancreatitis may provide objective data from which researchers could draw on to determine mairjuana’s effect on the development/severity of acute pancreatitis.
Disclosures:
Suhail Sidhu indicated no relevant financial relationships.
Walter Crum indicated no relevant financial relationships.
Omar Alaber indicated no relevant financial relationships.
Rahul Thusay indicated no relevant financial relationships.
Nikhil Furtado indicated no relevant financial relationships.
Ryan Walters indicated no relevant financial relationships.
Sandeep Mukherjee indicated no relevant financial relationships.
Suhail Sidhu, MD1, Walter Crum, MD2, Omar Alaber, MD2, Rahul Thusay, MA2, Nikhil Furtado, BS2, Ryan Walters, PhD2, Sandeep Mukherjee, MD2. P3495 - Association of Marijuana Use and the Severity of Idiopathic Acute Pancreatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
