Tuesday Poster Session
Category: Biliary/Pancreas
P3499 - Malignant Biliary Obstruction Due to Metastatic Urothelial Carcinoma
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Karin Estelle Mba Eya, MD
American Gastroenterological Association
Morristown, NJ
Presenting Author(s)
Karin Estelle Mba Eya, MD, Nnaemeka Anyadike, MD
American Gastroenterological Association, Morristown, NJ
Introduction: Malignant biliary obstruction is most often a result of primary neoplasms of the bile duct, gallbladder, liver, and pancreatic head. Metastasis from distant malignancies rarely causes biliary obstruction. Urothelial cancer (UC) is the most common histologic type of bladder cancer, accounting for 90% of cases. Lymph nodes, liver, lungs, bone, and peritoneum are the most common metastatic sites of UC. It is uncommon for UC to metastasize to the bile ducts. We present the case of an 86-year-old man with a history of UC who presented with biliary obstruction secondary to metastatic UC.
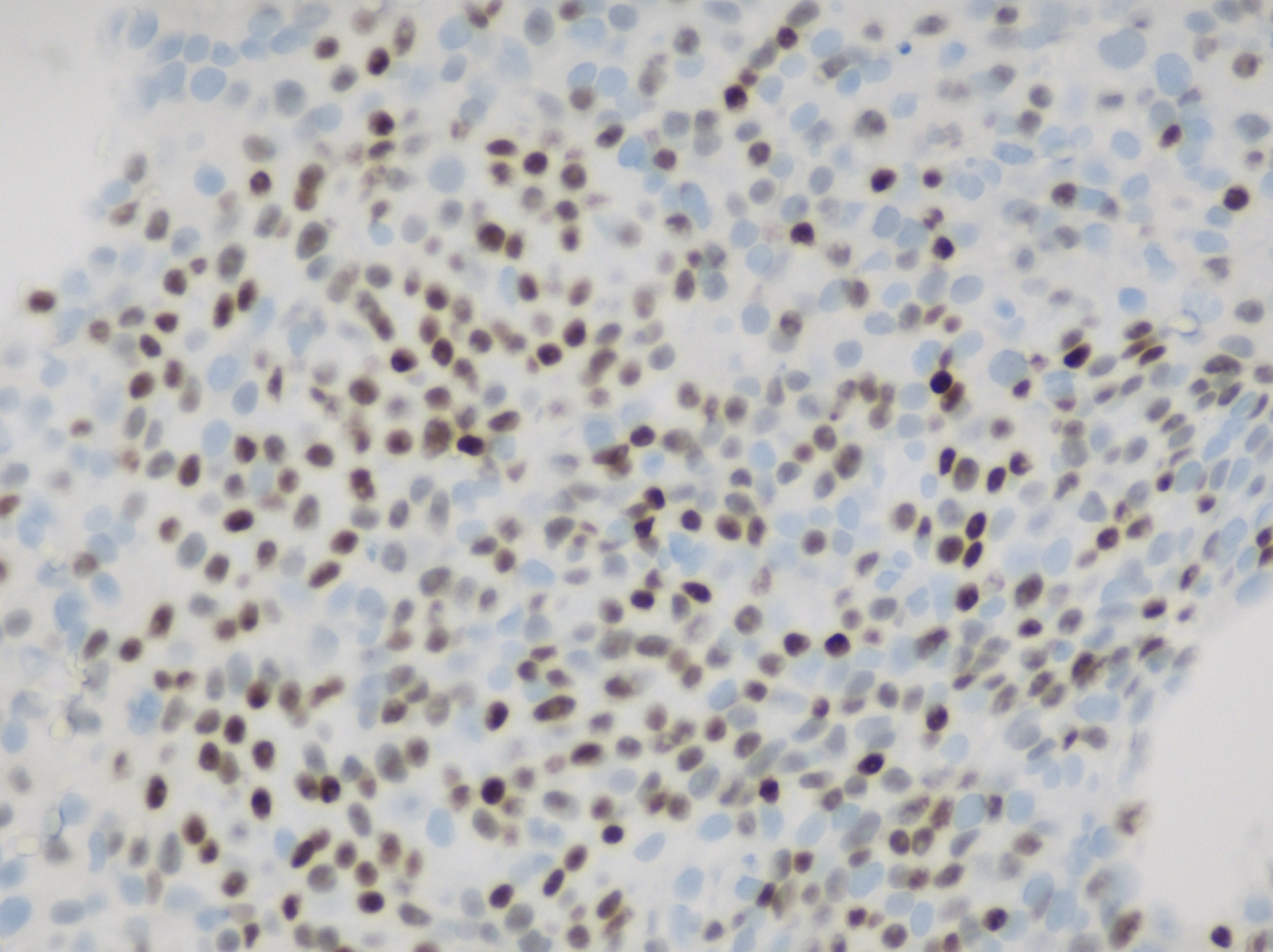
Case Description/Methods: An 86-year-old man with a past medical history of bladder cancer who presented to the emergency department for pruritus and jaundice. His physical exam was notable for scleral icterus. Initial laboratory results revealed elevated liver enzymes. Acute hepatitis B and A panel were negative. An abdominal ultrasound showed cholelithiasis and a dilated common bile duct (CBD) measuring 8 mm. An MRCP showed moderate dilation of the common hepatic duct and intrahepatic biliary ducts, and a filling defect was seen in the distal common hepatic bile duct suspicious for choledocholithiasis. Endoscopic ultrasound (EUS) was subsequently performed revealing a CBD wall thickening up to 4.4 mm with resulting stricture. Fine needle biopsy (FNB) was performed of the stricture. ERCP with cholangioscopy was notable for mucosal scarring and inflammation. Spybite biopsy and cytology were performed with the placement of a plastic biliary stent. Cytology brushing and spybite of the duct were non-diagnostic. Pathology from the FNB was consistent with metastatic urothelial carcinoma (Figure 1).
Discussion: Hepatobiliary metastasis of UC has been previously reported in the literature, however, only two cases of bile duct metastases have been documented. This is the third case of bile duct UC metastasis. One previously reported case is notable for non-diagnostic pathology from sampling during ERCP ultimately diagnosed during laparoscopic biopsy. However, in this case, a definitive diagnosis was made by FNB of the thickened bile duct wall. We hypothesize this discrepancy in diagnostic value may be explained by the lymphatic propagation of UC into the biliary tree. This case highlights the importance of including metastatic disease in the differential diagnosis of obstructive jaundice. Additionally, FNB should be a strongly considered modality for sampling obstructive bile duct tumors.
Disclosures:
Karin Estelle Mba Eya, MD, Nnaemeka Anyadike, MD. P3499 - Malignant Biliary Obstruction Due to Metastatic Urothelial Carcinoma, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
American Gastroenterological Association, Morristown, NJ
Introduction: Malignant biliary obstruction is most often a result of primary neoplasms of the bile duct, gallbladder, liver, and pancreatic head. Metastasis from distant malignancies rarely causes biliary obstruction. Urothelial cancer (UC) is the most common histologic type of bladder cancer, accounting for 90% of cases. Lymph nodes, liver, lungs, bone, and peritoneum are the most common metastatic sites of UC. It is uncommon for UC to metastasize to the bile ducts. We present the case of an 86-year-old man with a history of UC who presented with biliary obstruction secondary to metastatic UC.
Case Description/Methods: An 86-year-old man with a past medical history of bladder cancer who presented to the emergency department for pruritus and jaundice. His physical exam was notable for scleral icterus. Initial laboratory results revealed elevated liver enzymes. Acute hepatitis B and A panel were negative. An abdominal ultrasound showed cholelithiasis and a dilated common bile duct (CBD) measuring 8 mm. An MRCP showed moderate dilation of the common hepatic duct and intrahepatic biliary ducts, and a filling defect was seen in the distal common hepatic bile duct suspicious for choledocholithiasis. Endoscopic ultrasound (EUS) was subsequently performed revealing a CBD wall thickening up to 4.4 mm with resulting stricture. Fine needle biopsy (FNB) was performed of the stricture. ERCP with cholangioscopy was notable for mucosal scarring and inflammation. Spybite biopsy and cytology were performed with the placement of a plastic biliary stent. Cytology brushing and spybite of the duct were non-diagnostic. Pathology from the FNB was consistent with metastatic urothelial carcinoma (Figure 1).
Discussion: Hepatobiliary metastasis of UC has been previously reported in the literature, however, only two cases of bile duct metastases have been documented. This is the third case of bile duct UC metastasis. One previously reported case is notable for non-diagnostic pathology from sampling during ERCP ultimately diagnosed during laparoscopic biopsy. However, in this case, a definitive diagnosis was made by FNB of the thickened bile duct wall. We hypothesize this discrepancy in diagnostic value may be explained by the lymphatic propagation of UC into the biliary tree. This case highlights the importance of including metastatic disease in the differential diagnosis of obstructive jaundice. Additionally, FNB should be a strongly considered modality for sampling obstructive bile duct tumors.
Figure: Figure 1. Immunostaining image shows p40 positivity, although not specific for urothelial carcinoma, it also stains squamous cell carcinomas and should be negative in a primary adenocarcinoma/cholangiocarcinoma.
Disclosures:
Karin Estelle Mba Eya indicated no relevant financial relationships.
Nnaemeka Anyadike indicated no relevant financial relationships.
Karin Estelle Mba Eya, MD, Nnaemeka Anyadike, MD. P3499 - Malignant Biliary Obstruction Due to Metastatic Urothelial Carcinoma, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
