Tuesday Poster Session
Category: Biliary/Pancreas
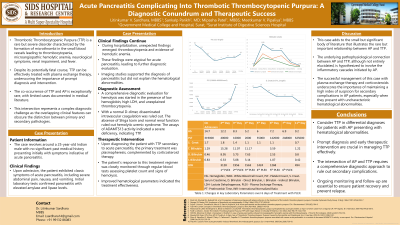
P3526 - Acute Pancreatitis Complicating Into Thrombotic Thrombocytopenic Purpura: A Diagnostic Conundrum and Therapeutic Success
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- LS
Litinkumar V. Sardhara, MBBS
Government Medical College and Hospital
Surat, Gujarat, India
Presenting Author(s)
Litinkumar V.. Sardhara, MBBS1, Sankalp Parikh, MBBS, MD2, Mipasha Patel, MBBS1, Meetkumar V.. Pipaliya, MBBS1, Rajiv Mehta, MBBS, MD3
1Government Medical College and Hospital, Surat, Gujarat, India; 2SIDS Hospital and Research Center, Surat, Gujarat, India; 3Surat Institute of Digestive Sciences Hospital, Surat, Gujarat, India
Introduction: A rare but serious condition known as thrombotic thrombocytopenic purpura (TTP) is characterized by the formation of microthrombi in small blood vessels, which can result in thrombocytopenia and microangiopathic hemolytic anemia. While some cases of acute pancreatitis have been observed as a consequence of TTP, occurrences of acute pancreatitis leading to TTP are seldom documented. This case illustrates this rare possibility of acute pancreatitis (AP) complicating into TTP, posing a significant diagnostic challenge.
Case Description/Methods: A 25-year-old Indian male patient with no significant medical history reported intense, non-radiating abdominal pain, nausea, and vomiting for one day. The elevated lipase and amylase levels confirmed the diagnosis of AP. Despite the standard care, the patient’s condition deteriorated. On the second day of symptoms onset, unexpected findings of thrombocytopenia and hemolytic anemia were observed. A comprehensive diagnostic evaluation for hemolysis was started in the presence of low hemoglobin, high LDH, and unexplained thrombocytopenia. With a normal D-dimer, disseminated intravascular coagulation was ruled out. The absence of Shiga toxin and normal renal function ruled out hemolytic uremic syndrome. The assays of ADAMTS13 activity indicated a severe deficiency, indicating TTP. The diagnosis of TTP secondary to acute pancreatitis was made, and treatment was initiated. Corticosteroid therapy was administered along with six cycles of plasma exchange therapy (PLEX) as the primary treatment. The patient's response was monitored through regular blood tests by assessing platelet count and signs of hemolysis. Improved hematological values indicated
the treatment effectiveness. A UTI developed during the hospitalization and treated effectively with fosfomycin.
Discussion: This case highlights the uncommon but significant complication of TTP arising from AP. Although the exact pathophysiological relationship is unknown, it most likely involves AP-initiated inflammatory cascades. The successful management of this patient underscores the importance of considering TTP in the differential diagnosis for AP patients with hematological abnormalities. While potentially fatal, TTP can be effectively treated with PLEX, emphasizing the need for prompt diagnosis and intervention. This case contributes to the limited literature on AP-induced TTP and underscores the need for thorough diagnostic approaches.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Litinkumar V.. Sardhara, MBBS1, Sankalp Parikh, MBBS, MD2, Mipasha Patel, MBBS1, Meetkumar V.. Pipaliya, MBBS1, Rajiv Mehta, MBBS, MD3. P3526 - Acute Pancreatitis Complicating Into Thrombotic Thrombocytopenic Purpura: A Diagnostic Conundrum and Therapeutic Success, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Government Medical College and Hospital, Surat, Gujarat, India; 2SIDS Hospital and Research Center, Surat, Gujarat, India; 3Surat Institute of Digestive Sciences Hospital, Surat, Gujarat, India
Introduction: A rare but serious condition known as thrombotic thrombocytopenic purpura (TTP) is characterized by the formation of microthrombi in small blood vessels, which can result in thrombocytopenia and microangiopathic hemolytic anemia. While some cases of acute pancreatitis have been observed as a consequence of TTP, occurrences of acute pancreatitis leading to TTP are seldom documented. This case illustrates this rare possibility of acute pancreatitis (AP) complicating into TTP, posing a significant diagnostic challenge.
Case Description/Methods: A 25-year-old Indian male patient with no significant medical history reported intense, non-radiating abdominal pain, nausea, and vomiting for one day. The elevated lipase and amylase levels confirmed the diagnosis of AP. Despite the standard care, the patient’s condition deteriorated. On the second day of symptoms onset, unexpected findings of thrombocytopenia and hemolytic anemia were observed. A comprehensive diagnostic evaluation for hemolysis was started in the presence of low hemoglobin, high LDH, and unexplained thrombocytopenia. With a normal D-dimer, disseminated intravascular coagulation was ruled out. The absence of Shiga toxin and normal renal function ruled out hemolytic uremic syndrome. The assays of ADAMTS13 activity indicated a severe deficiency, indicating TTP. The diagnosis of TTP secondary to acute pancreatitis was made, and treatment was initiated. Corticosteroid therapy was administered along with six cycles of plasma exchange therapy (PLEX) as the primary treatment. The patient's response was monitored through regular blood tests by assessing platelet count and signs of hemolysis. Improved hematological values indicated
the treatment effectiveness. A UTI developed during the hospitalization and treated effectively with fosfomycin.
Discussion: This case highlights the uncommon but significant complication of TTP arising from AP. Although the exact pathophysiological relationship is unknown, it most likely involves AP-initiated inflammatory cascades. The successful management of this patient underscores the importance of considering TTP in the differential diagnosis for AP patients with hematological abnormalities. While potentially fatal, TTP can be effectively treated with PLEX, emphasizing the need for prompt diagnosis and intervention. This case contributes to the limited literature on AP-induced TTP and underscores the need for thorough diagnostic approaches.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Litinkumar Sardhara indicated no relevant financial relationships.
Sankalp Parikh indicated no relevant financial relationships.
Mipasha Patel indicated no relevant financial relationships.
Meetkumar Pipaliya indicated no relevant financial relationships.
Rajiv Mehta indicated no relevant financial relationships.
Litinkumar V.. Sardhara, MBBS1, Sankalp Parikh, MBBS, MD2, Mipasha Patel, MBBS1, Meetkumar V.. Pipaliya, MBBS1, Rajiv Mehta, MBBS, MD3. P3526 - Acute Pancreatitis Complicating Into Thrombotic Thrombocytopenic Purpura: A Diagnostic Conundrum and Therapeutic Success, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
