Tuesday Poster Session
Category: Biliary/Pancreas
P3530 - Life-Threatening Gastrointestinal Bleeding due to Hemorrhagic Necrotizing Pancreatitis Complicated by a Colopancreatic Fistula
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Adamsegd I. Gebremedhen, MD
Marshall University Joan C. Edwards School of Medicine
Huntington, WV
Presenting Author(s)
Award: Presidential Poster Award
Adamsegd I. Gebremedhen, MD, Omar Al Metwali, MBBCh, Adnan Elghezewi, MD, Bassel Dakkak, MD, Abdelwahap Elghezewi, MBBCh, Wesam M. Frandah, MD
Marshall University Joan C. Edwards School of Medicine, Huntington, WV
Introduction: Necrotizing pancreatitis (NP) is a condition characterized by the presence of necrotic pancreatic parenchyma appearing as a significant nonenhanced section on computed tomography (CT). Colonic complications of NP include colonic necrosis, stricture, and fistula. Colonic fistula can present with fever, diarrhea, and hematochezia. We present a case of a 74-year-old white male who developed a life-threatening lower gastrointestinal (GI) bleeding from an NP complicated with a colopancreatic fistula (CPF).
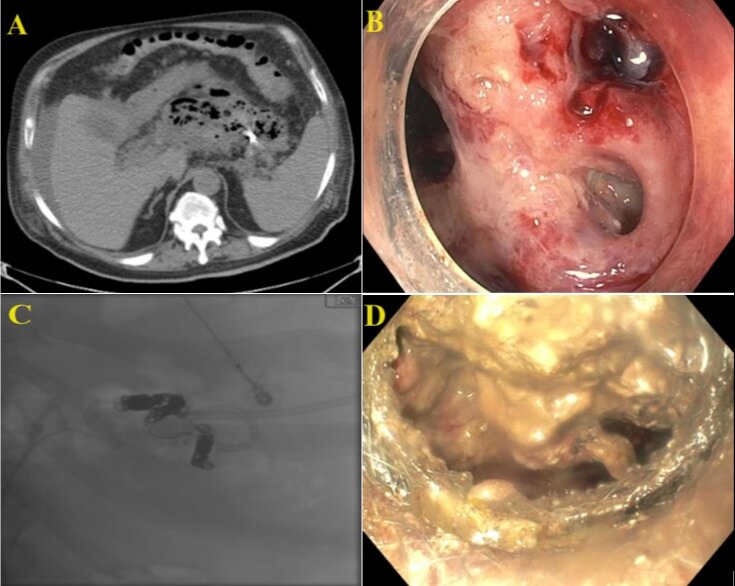
Case Description/Methods: A 74-year-old white male with a history of acute pancreatitis presented to an outside facility with episodes of bloody bowel movement. On presentation, he was hypotensive requiring resuscitation. His labs showed leukocytosis, low hemoglobin, and normal pancreatic enzyme levels. CT demonstrated necrotizing pancreatitis. He was transferred to our facility, admitted to the intensive care unit (ICU), and transfused with packed red blood cells (PRBC). CT with intravenous (IV) contrast demonstrated a splenic artery pseudoaneurysm and a large hemorrhagic pancreatic abscess (Figure A). He was started on broad-spectrum antibiotics. The Interventional radiology (IR) team embolized the splenic artery pseudoaneurysm and placed a pigtail catheter (Figure A). However, the episodes of bloody bowel movement continued. He then underwent a colonoscopy which revealed a fistula in the sigmoid colon communicating with retroperitoneal walled-off pancreatic necrosis and a bleeding vessel within the walled-off necrosis (Figure B). The IR team embolized the splenic artery across the pseudoaneurysm origin (Figure C). He then underwent cystogastrostomy stent placement (Figure D) and necrosectomy with repeat necrosectomy in four weeks.
Discussion: CPF in NP results from erosion and necrosis of the colonic wall from the activity of pancreatic enzymes, vascular thrombosis, and compromised blood flow. They commonly occur on the left side of the colon and present with abdominal pain, diarrhea, fever, nausea, and hematochezia. CPF are diagnosed with CT with IV contrast, CT with rectal contrast, contrast fistulography, and colonoscopy. CPF may spontaneously close by ensuring percutaneous drainage and infection control. Small-size CPF could be amenable to hemoclips, end loops, fibrin glue, and ligation bands. Large CPF, however, may require surgery. Our patient had an NP which was complicated by CPF and led to a life-threatening GI bleeding that was successfully managed conservatively.
Disclosures:
Adamsegd I. Gebremedhen, MD, Omar Al Metwali, MBBCh, Adnan Elghezewi, MD, Bassel Dakkak, MD, Abdelwahap Elghezewi, MBBCh, Wesam M. Frandah, MD. P3530 - Life-Threatening Gastrointestinal Bleeding due to Hemorrhagic Necrotizing Pancreatitis Complicated by a Colopancreatic Fistula, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Adamsegd I. Gebremedhen, MD, Omar Al Metwali, MBBCh, Adnan Elghezewi, MD, Bassel Dakkak, MD, Abdelwahap Elghezewi, MBBCh, Wesam M. Frandah, MD
Marshall University Joan C. Edwards School of Medicine, Huntington, WV
Introduction: Necrotizing pancreatitis (NP) is a condition characterized by the presence of necrotic pancreatic parenchyma appearing as a significant nonenhanced section on computed tomography (CT). Colonic complications of NP include colonic necrosis, stricture, and fistula. Colonic fistula can present with fever, diarrhea, and hematochezia. We present a case of a 74-year-old white male who developed a life-threatening lower gastrointestinal (GI) bleeding from an NP complicated with a colopancreatic fistula (CPF).
Case Description/Methods: A 74-year-old white male with a history of acute pancreatitis presented to an outside facility with episodes of bloody bowel movement. On presentation, he was hypotensive requiring resuscitation. His labs showed leukocytosis, low hemoglobin, and normal pancreatic enzyme levels. CT demonstrated necrotizing pancreatitis. He was transferred to our facility, admitted to the intensive care unit (ICU), and transfused with packed red blood cells (PRBC). CT with intravenous (IV) contrast demonstrated a splenic artery pseudoaneurysm and a large hemorrhagic pancreatic abscess (Figure A). He was started on broad-spectrum antibiotics. The Interventional radiology (IR) team embolized the splenic artery pseudoaneurysm and placed a pigtail catheter (Figure A). However, the episodes of bloody bowel movement continued. He then underwent a colonoscopy which revealed a fistula in the sigmoid colon communicating with retroperitoneal walled-off pancreatic necrosis and a bleeding vessel within the walled-off necrosis (Figure B). The IR team embolized the splenic artery across the pseudoaneurysm origin (Figure C). He then underwent cystogastrostomy stent placement (Figure D) and necrosectomy with repeat necrosectomy in four weeks.
Discussion: CPF in NP results from erosion and necrosis of the colonic wall from the activity of pancreatic enzymes, vascular thrombosis, and compromised blood flow. They commonly occur on the left side of the colon and present with abdominal pain, diarrhea, fever, nausea, and hematochezia. CPF are diagnosed with CT with IV contrast, CT with rectal contrast, contrast fistulography, and colonoscopy. CPF may spontaneously close by ensuring percutaneous drainage and infection control. Small-size CPF could be amenable to hemoclips, end loops, fibrin glue, and ligation bands. Large CPF, however, may require surgery. Our patient had an NP which was complicated by CPF and led to a life-threatening GI bleeding that was successfully managed conservatively.
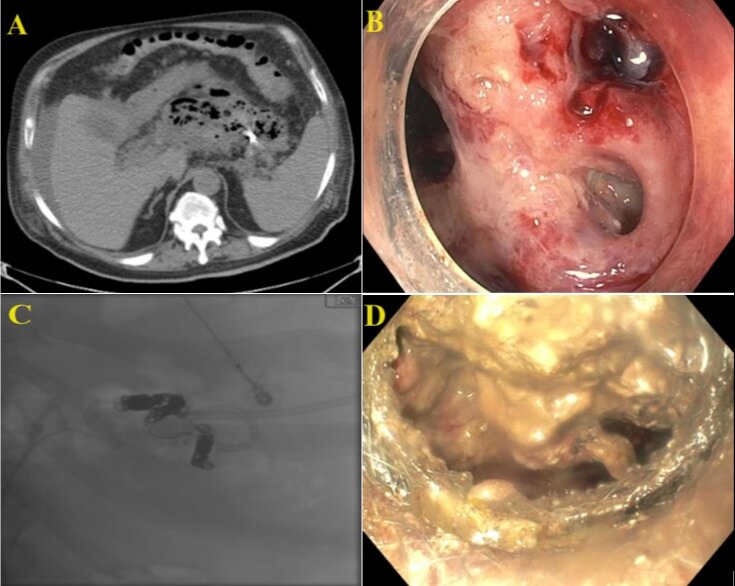
Figure: Figure A. Hemorrhagic pancreatic abscess with abscess drain. Figure B. Fistula in the sigmoid colon communicating with retroperitoneal walled-off pancreatic necrosis with bleeding vessel seen within the walled-off necrosis. Figure C. Splenic artery embolization across the origin of the pseudoaneurysm. Figure D. Cystogastrostomy stent
Disclosures:
Adamsegd Gebremedhen indicated no relevant financial relationships.
Omar Al Metwali indicated no relevant financial relationships.
Adnan Elghezewi indicated no relevant financial relationships.
Bassel Dakkak indicated no relevant financial relationships.
Abdelwahap Elghezewi indicated no relevant financial relationships.
Wesam Frandah: Endogastric solution – Consultant.
Adamsegd I. Gebremedhen, MD, Omar Al Metwali, MBBCh, Adnan Elghezewi, MD, Bassel Dakkak, MD, Abdelwahap Elghezewi, MBBCh, Wesam M. Frandah, MD. P3530 - Life-Threatening Gastrointestinal Bleeding due to Hemorrhagic Necrotizing Pancreatitis Complicated by a Colopancreatic Fistula, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.


