Tuesday Poster Session
Category: Biliary/Pancreas
P3542 - The Role of GLP-1 Agonist in Acute Cholecystitis After a Routine Colonoscopy: A Case Report
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Ahmad Mohammad Abdulraheem, MD
MedStar Health-Georgetown/Washington Hospital Center
Washington, DC
Presenting Author(s)
Ahmad Mohammad Abdulraheem, MD1, Usman Afzal, MD2, Dania Qarkash, MD3, Nadera Altork, MD1, Mohammed Abu-Rumaileh, MD4, Alireza Meighani, MD5
1MedStar Health-Georgetown/Washington Hospital Center, Washington, DC; 2Washington Hospital Center, Washington, DC; 3University of Jordan School of Medicine, Washington, DC; 4University of Toledo, Toledo, OH; 5MedStar Health, Washington Hospital Center, Washington, DC
Introduction: Colonoscopy (CLN) is a commonly performed low-risk gastroenterology procedure for diagnostic and therapeutic interventions, rarely resulting in serious complications. However, patients presenting with abdominal pain and vomiting after a CLN require detailed investigation to rule out acute abdomen emergencies such as bowel perforation, splenic rupture, or bleeding(1) . Acute cholecystitis (AC) is a rarely reported post-procedural complication(2) . Multiple theories have been proposed to explain this, although the mechanism remains unknown, such presentations can occur within the first 48-72 hours.
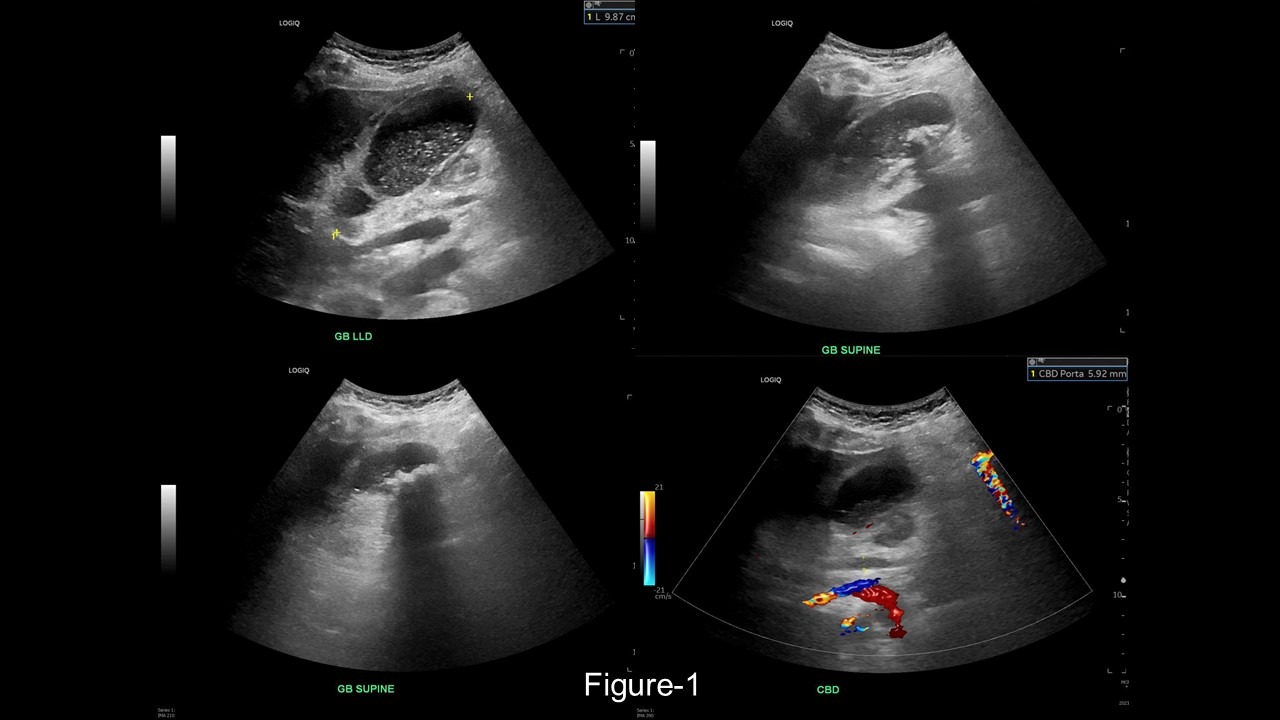
Case Description/Methods: A 66-year-old female with obesity, on semaglutide (Wegovy) 2.4 mg weekly, presented with abdominal pain one day after a screening CLN with rectal biopsies due to a small white patch. She had withheld her semaglutide dose one week prior due to its potential to cause delayed gastric emptying. Labs showed leukocytosis with a neutrophilic shift and unremarkable liver function tests and urine analysis. A CT abdomen with contrast indicated mild intrahepatic biliary ductal dilatation, a distended gallbladder, gallstones, and extensive pericholecystic fat stranding, suggestive of AC. An abdominal ultrasound showed no CBD dilatation: 0.6cm, however, confirmed a moderately distended gallbladder with stones, sludge, diffuse wall edema, trace pericholecystic fluid(Figure-1), and a positive sonographic Murphy sign. She was started on IV broad-spectrum antibiotics, consulted general surgery for AC, and underwent a cholecystectomy.
Discussion: In a systematic review and meta-analysis of randomized controlled trials(3), the findings indicated an elevated risk of gallbladder or biliary diseases associated with GLP-1 agonist use, especially at higher doses, for extended durations, and for weight loss purposes (He et al.). The proposed mechanism involves GLP-1 agonists inhibiting gallbladder motility and delaying gallbladder emptying through a direct effect on cholecystokinin inhibition (He et al.). Although our patient ceased taking semaglutide one week before the procedure, she still developed AC.
Conclusion: This suggests that while AC after a CLN is typically rare, its occurrence might be heightened by recent GLP-1 agonist use, particularly semaglutide due to its one-week half-life. Future studies are necessary to determine the optimal washout period for these medications before colonoscopies to minimize the risk of acute cholecystitis following these procedures.
Disclosures:
Ahmad Mohammad Abdulraheem, MD1, Usman Afzal, MD2, Dania Qarkash, MD3, Nadera Altork, MD1, Mohammed Abu-Rumaileh, MD4, Alireza Meighani, MD5. P3542 - The Role of GLP-1 Agonist in Acute Cholecystitis After a Routine Colonoscopy: A Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1MedStar Health-Georgetown/Washington Hospital Center, Washington, DC; 2Washington Hospital Center, Washington, DC; 3University of Jordan School of Medicine, Washington, DC; 4University of Toledo, Toledo, OH; 5MedStar Health, Washington Hospital Center, Washington, DC
Introduction: Colonoscopy (CLN) is a commonly performed low-risk gastroenterology procedure for diagnostic and therapeutic interventions, rarely resulting in serious complications. However, patients presenting with abdominal pain and vomiting after a CLN require detailed investigation to rule out acute abdomen emergencies such as bowel perforation, splenic rupture, or bleeding(1) . Acute cholecystitis (AC) is a rarely reported post-procedural complication(2) . Multiple theories have been proposed to explain this, although the mechanism remains unknown, such presentations can occur within the first 48-72 hours.
Case Description/Methods: A 66-year-old female with obesity, on semaglutide (Wegovy) 2.4 mg weekly, presented with abdominal pain one day after a screening CLN with rectal biopsies due to a small white patch. She had withheld her semaglutide dose one week prior due to its potential to cause delayed gastric emptying. Labs showed leukocytosis with a neutrophilic shift and unremarkable liver function tests and urine analysis. A CT abdomen with contrast indicated mild intrahepatic biliary ductal dilatation, a distended gallbladder, gallstones, and extensive pericholecystic fat stranding, suggestive of AC. An abdominal ultrasound showed no CBD dilatation: 0.6cm, however, confirmed a moderately distended gallbladder with stones, sludge, diffuse wall edema, trace pericholecystic fluid(Figure-1), and a positive sonographic Murphy sign. She was started on IV broad-spectrum antibiotics, consulted general surgery for AC, and underwent a cholecystectomy.
Discussion: In a systematic review and meta-analysis of randomized controlled trials(3), the findings indicated an elevated risk of gallbladder or biliary diseases associated with GLP-1 agonist use, especially at higher doses, for extended durations, and for weight loss purposes (He et al.). The proposed mechanism involves GLP-1 agonists inhibiting gallbladder motility and delaying gallbladder emptying through a direct effect on cholecystokinin inhibition (He et al.). Although our patient ceased taking semaglutide one week before the procedure, she still developed AC.
Conclusion: This suggests that while AC after a CLN is typically rare, its occurrence might be heightened by recent GLP-1 agonist use, particularly semaglutide due to its one-week half-life. Future studies are necessary to determine the optimal washout period for these medications before colonoscopies to minimize the risk of acute cholecystitis following these procedures.
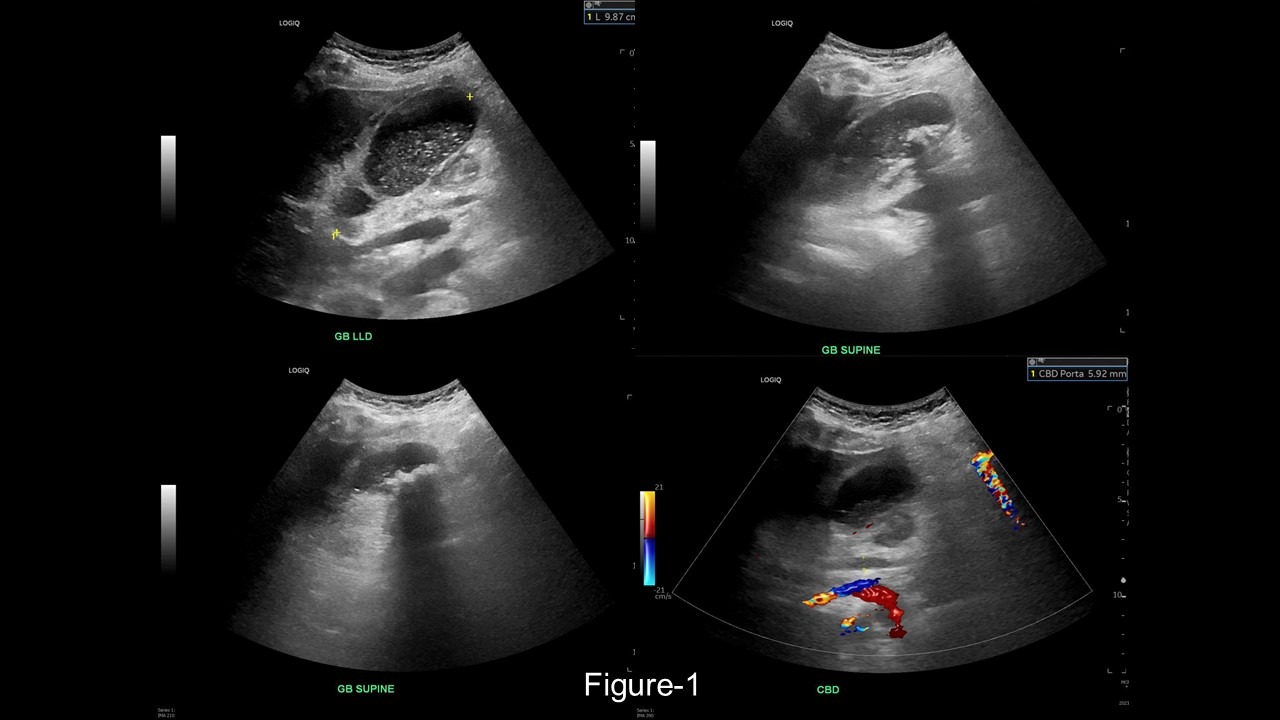
Figure: US findings of acute cholecystitis
Disclosures:
Ahmad Mohammad Abdulraheem indicated no relevant financial relationships.
Usman Afzal indicated no relevant financial relationships.
Dania Qarkash indicated no relevant financial relationships.
Nadera Altork indicated no relevant financial relationships.
Mohammed Abu-Rumaileh indicated no relevant financial relationships.
Alireza Meighani indicated no relevant financial relationships.
Ahmad Mohammad Abdulraheem, MD1, Usman Afzal, MD2, Dania Qarkash, MD3, Nadera Altork, MD1, Mohammed Abu-Rumaileh, MD4, Alireza Meighani, MD5. P3542 - The Role of GLP-1 Agonist in Acute Cholecystitis After a Routine Colonoscopy: A Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

