Tuesday Poster Session
Category: Biliary/Pancreas
P3543 - An Atypical Presentation of Coexisting Pancreatic and Ovarian Cysts
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E

Has Audio
- AN
Antoine Nguyen
University of North Texas Health Science Center
Houston, TX
Presenting Author(s)
Antoine Nguyen, 1, Jesus Tamayo, 2, Swetha Paluru, MD3
1University of North Texas Health Science Center, Houston, TX; 2University of North Texas Health Science Center, Fort Worth, TX; 3John Peter Smith Hospital, Fort Worth, TX
Introduction: Pancreatic cystic neoplasms (PCNs) often present asymptomatically or nonspecifically in patients and are frequently discovered incidentally on imaging. Serous PCNs typically do not require further evaluation as they have virtually negligible risk for malignancy. In contrast, mucinous PCNs have moderate risk for malignant potential in up to 38% of cases.1 Consequently, mucinous PCNs usually warrant further evaluation with endoscopic ultrasound-guided fine-needle aspiration (EUS-FNA) for cytopathologic evaluation.2
Case Description/Methods: A 29-year-old female with a past medical history of non-alcoholic fatty liver disease was found to have a large cystic lesion in the tail of the pancreas with extension into the retroperitoneum. The patient underwent EUS-FNA for histologic assessment. Notable labs include amylase >1,300 (normal: 25 - 115 U/L), CEA of 0.5 (normal ≤ 2.5 ng/mL), and CA 19-9 of 20 (normal: ≤ 35 U/mL). She denied family history of colon, pancreatic, or ovarian adenocarcinoma. Additionally, she was found to have a large 11 cm para-tubal left ovarian serous cyst.
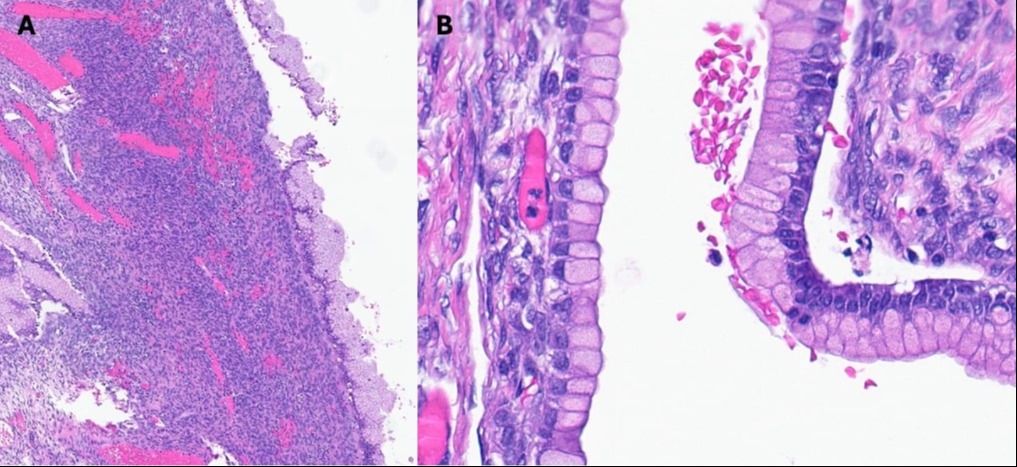
Robotic-assisted laparoscopic subtotal distal pancreatectomy with concurrent partial salpingectomy and oophorectomy was performed without complication. The mucinous PCN demonstrated a background of chronic pancreatitis with islet cell hyperplasia (Fig 1). This was histologically consistent with mucus cystic neoplasm as it demonstrated dense ovarian stroma with immunohistochemistry staining positive for CD10 and estrogen receptor (Fig 2). The ovarian cyst was consistent with serous cystadenoma and histologically unremarkable.
Discussion: Mucinous PCNs are not uncommon as they represent approximately 23% of PCNs.2 Most present in the 5th to 7th decade of life and almost exclusively affect females.3 This case of mucinous PCN is remarkable due to its large size and presentation in a much younger patient. Both cysts in this patient appeared clinically and histologically benign. However, the coexisting pancreatic and ovarian masses justified the concern and risk for malignant transformation. Thus, it was appropriate to undergo surgical resection and obtain CA 19-9 and CEA levels for baseline monitoring. Characteristics that have been associated with malignant transformation of mucinous PCNs include size greater than 5 cm, solid mass component, and irregular cyst wall thickening or calcification.1 KRAS, GNAS, TP53, PTEN, and PIK3CA are mutations that have been implicated in malignant cases of mucinous PCNs.4
Disclosures:
Antoine Nguyen, 1, Jesus Tamayo, 2, Swetha Paluru, MD3. P3543 - An Atypical Presentation of Coexisting Pancreatic and Ovarian Cysts, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of North Texas Health Science Center, Houston, TX; 2University of North Texas Health Science Center, Fort Worth, TX; 3John Peter Smith Hospital, Fort Worth, TX
Introduction: Pancreatic cystic neoplasms (PCNs) often present asymptomatically or nonspecifically in patients and are frequently discovered incidentally on imaging. Serous PCNs typically do not require further evaluation as they have virtually negligible risk for malignancy. In contrast, mucinous PCNs have moderate risk for malignant potential in up to 38% of cases.1 Consequently, mucinous PCNs usually warrant further evaluation with endoscopic ultrasound-guided fine-needle aspiration (EUS-FNA) for cytopathologic evaluation.2
Case Description/Methods: A 29-year-old female with a past medical history of non-alcoholic fatty liver disease was found to have a large cystic lesion in the tail of the pancreas with extension into the retroperitoneum. The patient underwent EUS-FNA for histologic assessment. Notable labs include amylase >1,300 (normal: 25 - 115 U/L), CEA of 0.5 (normal ≤ 2.5 ng/mL), and CA 19-9 of 20 (normal: ≤ 35 U/mL). She denied family history of colon, pancreatic, or ovarian adenocarcinoma. Additionally, she was found to have a large 11 cm para-tubal left ovarian serous cyst.
Robotic-assisted laparoscopic subtotal distal pancreatectomy with concurrent partial salpingectomy and oophorectomy was performed without complication. The mucinous PCN demonstrated a background of chronic pancreatitis with islet cell hyperplasia (Fig 1). This was histologically consistent with mucus cystic neoplasm as it demonstrated dense ovarian stroma with immunohistochemistry staining positive for CD10 and estrogen receptor (Fig 2). The ovarian cyst was consistent with serous cystadenoma and histologically unremarkable.
Discussion: Mucinous PCNs are not uncommon as they represent approximately 23% of PCNs.2 Most present in the 5th to 7th decade of life and almost exclusively affect females.3 This case of mucinous PCN is remarkable due to its large size and presentation in a much younger patient. Both cysts in this patient appeared clinically and histologically benign. However, the coexisting pancreatic and ovarian masses justified the concern and risk for malignant transformation. Thus, it was appropriate to undergo surgical resection and obtain CA 19-9 and CEA levels for baseline monitoring. Characteristics that have been associated with malignant transformation of mucinous PCNs include size greater than 5 cm, solid mass component, and irregular cyst wall thickening or calcification.1 KRAS, GNAS, TP53, PTEN, and PIK3CA are mutations that have been implicated in malignant cases of mucinous PCNs.4
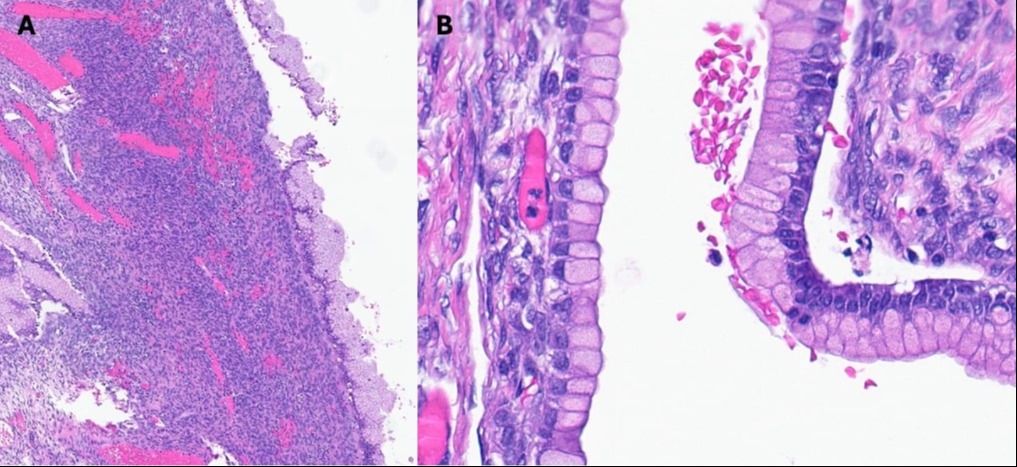
Figure: Figure 1A – A multiloculated 6.5 cm cyst containing viscous, gelatinous fluid is demonstrated on distal pancreatectomy specimen. Background pancreas showed chronic pancreatitis and islet cell hyperplasia.
Figure 1B – Microscopically, the cyst is lined with foveolar mucinous epithelium surrounded by dense ovarian type stroma that demonstrate variable atypia and low-grade dysplasia. The ovarian stroma is positive for CD10 and Estrogen receptor by immunohistochemistry.
Figure 1B – Microscopically, the cyst is lined with foveolar mucinous epithelium surrounded by dense ovarian type stroma that demonstrate variable atypia and low-grade dysplasia. The ovarian stroma is positive for CD10 and Estrogen receptor by immunohistochemistry.
Disclosures:
Antoine Nguyen indicated no relevant financial relationships.
Jesus Tamayo indicated no relevant financial relationships.
Swetha Paluru indicated no relevant financial relationships.
Antoine Nguyen, 1, Jesus Tamayo, 2, Swetha Paluru, MD3. P3543 - An Atypical Presentation of Coexisting Pancreatic and Ovarian Cysts, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
