Tuesday Poster Session
Category: Biliary/Pancreas
P3551 - Ouch That Hurts! Pancreatic Panniculitis Secondary to Chronic Pancreatitis in a Patient With Monoallelic CFTR Mutation
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Tinsa Varughese, DO
Lehigh Valley Health Network
Allentown, PA
Presenting Author(s)
Tinsa Varughese, DO, Amanda Jacubowsky, DO, Lei Li, MD, MS
Lehigh Valley Health Network, Allentown, PA
Introduction: Pancreatic panniculitis is a rare skin manifestation occurring in about 2-3% of patients with acute pancreatitis, chronic pancreatitis, or pancreatic cancer. Patients can present with tender, ulcerated, and violaceous nodules on their upper and lower extremities along with fever, weight loss, and joint manifestations. Here, we present a unique case of a patient with a monoallelic cystic fibrosis transmembrane conductance regulator (CFTR) mutation who was found to have pancreatic panniculitis.
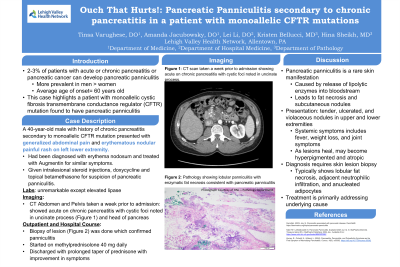
Case Description/Methods: A 40 year-old-male with a past medical history of monoallelic CFTR mutation complicated by chronic pancreatitis presented to the hospital with generalized abdominal pain and an erythematous, nodular, painful, rash on his left leg. The patient was previously seen a week prior by his general practitioner for similar symptoms, was diagnosed with erythema nodosum, and was prescribed augmentin. Without improvement in his rash, he was seen by his outpatient gastroenterologist who suspected pancreatic panniculitis. The patient underwent intralesional steroid injections with dermatology and was prescribed doxycycline and topical betamethasone. Due to acute worsening of his symptoms, the patient was admitted to the hospital for further workup. His pain was refractory to opioids, and subsequently he was started on methylprednisolone 40 mg daily. A biopsy of his skin lesions were consistent with panniculitis. The patient was later discharged on a prolonged taper of prednisone starting at 60 mg daily which improved his symptoms.
Discussion: Pancreatic panniculitis is caused by the release of lipolytic enzymes into the bloodstream that leads to fat necrosis and subcutaneous nodules. It is four times more prevalent in men than women with an average age of onset around 60 years old. Evaluation in patients suspected of pancreatic panniculitis requires thorough physical exam, complete blood counts, lipase, amylase, transaminase, bilirubin, and inflammatory markers. CT scans of the abdomen and pelvis with contrast can be used to evaluate for a pancreatic etiology. A biopsy of skin lesions is required for diagnosis of pancreatic panniculitis with findings such as lobular fat necrosis, adjacent neutrophilic infiltration, and anucleated adipocytes also known as ghost adipocytes. The treatment is to address the underlying cause, however, as nodules heal, they may leave behind hyperpigmented, atrophic scarring.
Disclosures:
Tinsa Varughese, DO, Amanda Jacubowsky, DO, Lei Li, MD, MS. P3551 - Ouch That Hurts! Pancreatic Panniculitis Secondary to Chronic Pancreatitis in a Patient With Monoallelic CFTR Mutation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Lehigh Valley Health Network, Allentown, PA
Introduction: Pancreatic panniculitis is a rare skin manifestation occurring in about 2-3% of patients with acute pancreatitis, chronic pancreatitis, or pancreatic cancer. Patients can present with tender, ulcerated, and violaceous nodules on their upper and lower extremities along with fever, weight loss, and joint manifestations. Here, we present a unique case of a patient with a monoallelic cystic fibrosis transmembrane conductance regulator (CFTR) mutation who was found to have pancreatic panniculitis.
Case Description/Methods: A 40 year-old-male with a past medical history of monoallelic CFTR mutation complicated by chronic pancreatitis presented to the hospital with generalized abdominal pain and an erythematous, nodular, painful, rash on his left leg. The patient was previously seen a week prior by his general practitioner for similar symptoms, was diagnosed with erythema nodosum, and was prescribed augmentin. Without improvement in his rash, he was seen by his outpatient gastroenterologist who suspected pancreatic panniculitis. The patient underwent intralesional steroid injections with dermatology and was prescribed doxycycline and topical betamethasone. Due to acute worsening of his symptoms, the patient was admitted to the hospital for further workup. His pain was refractory to opioids, and subsequently he was started on methylprednisolone 40 mg daily. A biopsy of his skin lesions were consistent with panniculitis. The patient was later discharged on a prolonged taper of prednisone starting at 60 mg daily which improved his symptoms.
Discussion: Pancreatic panniculitis is caused by the release of lipolytic enzymes into the bloodstream that leads to fat necrosis and subcutaneous nodules. It is four times more prevalent in men than women with an average age of onset around 60 years old. Evaluation in patients suspected of pancreatic panniculitis requires thorough physical exam, complete blood counts, lipase, amylase, transaminase, bilirubin, and inflammatory markers. CT scans of the abdomen and pelvis with contrast can be used to evaluate for a pancreatic etiology. A biopsy of skin lesions is required for diagnosis of pancreatic panniculitis with findings such as lobular fat necrosis, adjacent neutrophilic infiltration, and anucleated adipocytes also known as ghost adipocytes. The treatment is to address the underlying cause, however, as nodules heal, they may leave behind hyperpigmented, atrophic scarring.
Disclosures:
Tinsa Varughese indicated no relevant financial relationships.
Amanda Jacubowsky indicated no relevant financial relationships.
Lei Li indicated no relevant financial relationships.
Tinsa Varughese, DO, Amanda Jacubowsky, DO, Lei Li, MD, MS. P3551 - Ouch That Hurts! Pancreatic Panniculitis Secondary to Chronic Pancreatitis in a Patient With Monoallelic CFTR Mutation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
