Tuesday Poster Session
Category: Biliary/Pancreas
P3557 - Segmental Arterial Mediolysis With Hepatic Artery Aneurysm Causing Biliary Obstruction and Arterio-Biliary Fistula: Rare Presentation of a Rare Disease
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Jenson Phung, MD
University of Minnesota
Minneapolis, MN
Presenting Author(s)
Award: Presidential Poster Award
Jenson Phung, MD1, Rahul Karna, MD1, Guru Trikudanathan, MD1, Nabeel Azeem, MD2
1University of Minnesota, Minneapolis, MN; 2University of Minnesota Medical Center, Minneapolis, MN
Introduction: Segmental arterial mediolysis (SAM) is a rare non-atherosclerotic, non-hereditary, and non-inflammatory condition that predominantly affects the splanchnic vasculature. Damage to the arterial wall can lead to aneurysms, dissection, or bleeding. Here we present a case of SAM involving the hepatic artery causing biliary obstruction and arterio-biliary fistula.
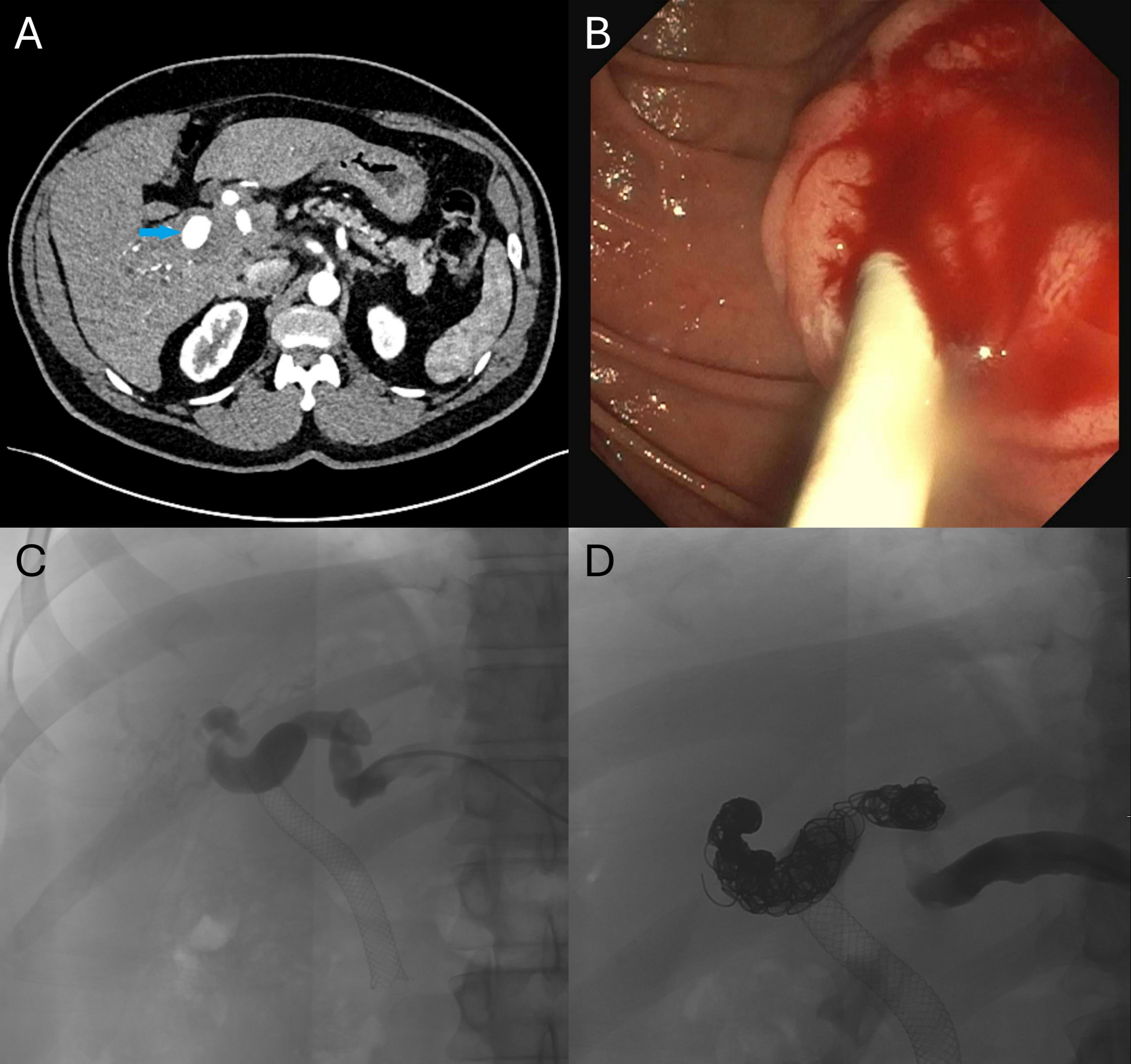
Case Description/Methods: A 42-year-old male with history of tobacco use presented with abdominal pain. He was hypertensive and had elevated liver enzymes. Computed tomography angiography (CTA) of the abdomen revealed a 17 mm right hepatic artery aneurysm. Infectious, atherosclerotic, and inflammatory etiologies were ruled out. After comprehensive evaluations from the multidisciplinary team, he was diagnosed with SAM.
Three months later, the patient was readmitted with dark urine, pale stools, and new direct hyperbilirubinemia. CTA showed stable appearance of his hepatic artery aneurysm but dilation of the intrahepatic bile ducts due to mass effect from his aneurysm. He underwent endoscopic retrograde cholangiopancreatography (ERCP) showing a common hepatic duct stricture secondary to extrinsic compression from hepatic artery aneurysm. 7 Fr biliary stents were placed across the area of stricture.
The patient re-presented later with bright red blood per rectum and hematemesis, concerning for a brisk upper GI bleed. Due to concomitant chills and leukocytosis, an urgent ERCP was performed. His prior stents were in stable position but were now occluded with clot. Removal of the stents was met with rapid pulsatile bleeding, suspicious for an arterial bleed. Opacification of the biliary tree was not achieved due to efflux of contrast from hemobilia. The pattern of bleeding was highly concerning for an arterio-biliary fistula from the known hepatic artery aneurysm. A 10 mm x 8 cm fully covered metal stent was placed across the common hepatic and common bile ducts, which led to cessation of bleeding and passage of bile through the stent. The patient then underwent coil embolization of the aneurysm by IR, with CTA the following day showing total thrombosis of the hepatic artery.
Discussion: SAM can present as obstructive jaundice from biliary obstruction or as bleeding from an arterio-biliary fistula. Prompt recognition of the presentation is key to successful management of complications of SAM. In our non-cirrhotic patient, hepatic perfusion remains intact after hepatic artery embolization due to delivery of oxygenated blood from the portal vein.
Disclosures:
Jenson Phung, MD1, Rahul Karna, MD1, Guru Trikudanathan, MD1, Nabeel Azeem, MD2. P3557 - Segmental Arterial Mediolysis With Hepatic Artery Aneurysm Causing Biliary Obstruction and Arterio-Biliary Fistula: Rare Presentation of a Rare Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Jenson Phung, MD1, Rahul Karna, MD1, Guru Trikudanathan, MD1, Nabeel Azeem, MD2
1University of Minnesota, Minneapolis, MN; 2University of Minnesota Medical Center, Minneapolis, MN
Introduction: Segmental arterial mediolysis (SAM) is a rare non-atherosclerotic, non-hereditary, and non-inflammatory condition that predominantly affects the splanchnic vasculature. Damage to the arterial wall can lead to aneurysms, dissection, or bleeding. Here we present a case of SAM involving the hepatic artery causing biliary obstruction and arterio-biliary fistula.
Case Description/Methods: A 42-year-old male with history of tobacco use presented with abdominal pain. He was hypertensive and had elevated liver enzymes. Computed tomography angiography (CTA) of the abdomen revealed a 17 mm right hepatic artery aneurysm. Infectious, atherosclerotic, and inflammatory etiologies were ruled out. After comprehensive evaluations from the multidisciplinary team, he was diagnosed with SAM.
Three months later, the patient was readmitted with dark urine, pale stools, and new direct hyperbilirubinemia. CTA showed stable appearance of his hepatic artery aneurysm but dilation of the intrahepatic bile ducts due to mass effect from his aneurysm. He underwent endoscopic retrograde cholangiopancreatography (ERCP) showing a common hepatic duct stricture secondary to extrinsic compression from hepatic artery aneurysm. 7 Fr biliary stents were placed across the area of stricture.
The patient re-presented later with bright red blood per rectum and hematemesis, concerning for a brisk upper GI bleed. Due to concomitant chills and leukocytosis, an urgent ERCP was performed. His prior stents were in stable position but were now occluded with clot. Removal of the stents was met with rapid pulsatile bleeding, suspicious for an arterial bleed. Opacification of the biliary tree was not achieved due to efflux of contrast from hemobilia. The pattern of bleeding was highly concerning for an arterio-biliary fistula from the known hepatic artery aneurysm. A 10 mm x 8 cm fully covered metal stent was placed across the common hepatic and common bile ducts, which led to cessation of bleeding and passage of bile through the stent. The patient then underwent coil embolization of the aneurysm by IR, with CTA the following day showing total thrombosis of the hepatic artery.
Discussion: SAM can present as obstructive jaundice from biliary obstruction or as bleeding from an arterio-biliary fistula. Prompt recognition of the presentation is key to successful management of complications of SAM. In our non-cirrhotic patient, hepatic perfusion remains intact after hepatic artery embolization due to delivery of oxygenated blood from the portal vein.
Figure: Figure 1. (A) Hepatic artery aneurysm as seen on computed tomography angiogram (blue arrow). (B) Endoscopic image showing blood from the biliary tract entering into the duodenum. (C) Angiogram of hepatic artery aneurysm prior to coil embolization. The patient’s biliary stent can also be seen in this view. (D) Angiogram of hepatic artery aneurysm immediately after successful placement of coils.
Disclosures:
Jenson Phung indicated no relevant financial relationships.
Rahul Karna indicated no relevant financial relationships.
Guru Trikudanathan: AbbVie – Grant/Research Support. Boston Scientific – Consultant.
Nabeel Azeem: Boston Scientific – Consultant.
Jenson Phung, MD1, Rahul Karna, MD1, Guru Trikudanathan, MD1, Nabeel Azeem, MD2. P3557 - Segmental Arterial Mediolysis With Hepatic Artery Aneurysm Causing Biliary Obstruction and Arterio-Biliary Fistula: Rare Presentation of a Rare Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

