Tuesday Poster Session
Category: Biliary/Pancreas
P3566 - Managing Disrupted Pancreatic Duct Syndrome With a Multimodal Endoscopic Approach
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Omar T. Ahmed, MD
University of Illinois at Chicago
Chicago, IL
Presenting Author(s)
Omar T. Ahmed, MD1, Kashif Osmani, MD1, Michael Gianarakis, MD1, Islam Mohamed, MD2, Ashley A. Vareedayah, MD1
1University of Illinois at Chicago, Chicago, IL; 2University of Missouri - Kansas City School of Medicine, Kansas City, MO
Introduction: Disrupted pancreatic duct syndrome (DrPDS) involves a partial interruption of the pancreatic duct (PD), resulting from severe necrotizing pancreatitis. It is challenging to diagnose, requiring ERCP for confirmation. This case highlights the complexities and endoscopic management strategies for DrPDS.
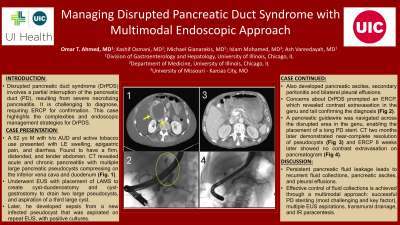
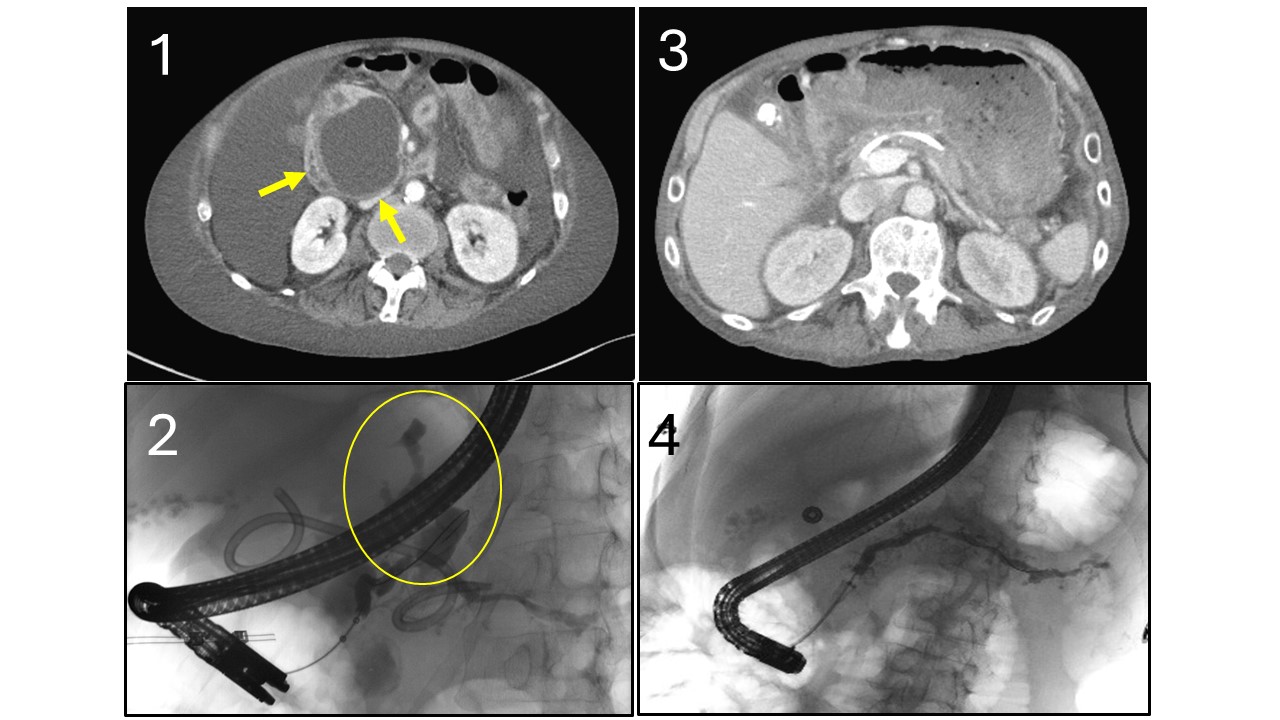
Case Description/Methods: A 62-year-old male with a history of alcohol use disorder and active tobacco use presented with lower extremity swelling, abdominal pain, and diarrhea. The patient was afebrile and tachycardic with a cachectic appearance and a firm, distended, and tender abdomen. Labs showed leukocytosis, mildly elevated lipase, and new AKI. CT abdomen/pelvis (CTAP) revealed acute and chronic pancreatitis with multiple large pancreatic pseudocysts compressing on the inferior vena cava and duodenum (Fig. 1).
The patient underwent endoscopic ultrasound (EUS) with placement of lumen-apposing metal stents to create cyst-duodenostomy and cyst-gastrostomy to drain two large pseudocysts, and aspirated a third large cyst. Despite initially stabilizing, the patient developed sepsis from a new, infected pseudocyst that was aspirated on repeat EUS, and cultures grew candida Krusei and tropicalis and E. facium. The patient also developed pancreatic ascites with secondary peritonitis and bilateral pleural effusions. Concerns about DrPDS prompted an ERCP, which revealed contrast extravasation in the genu and tail areas on the pancreatogram, confirming the diagnosis (Fig. 2). A pancreatic guidewire was navigated across the disrupted area in the genu, enabling the placement of a long pancreatic duct stent. CTAP two months later demonstrated near-complete resolution of pseudocysts (Fig. 3) and ERCP 8 weeks later showed no contrast extravasation on pancreatogram (Fig. 4).
Discussion: In DrPDS, persistent pancreatic fluid leakage leads to recurrent fluid collections, pseudocysts, pancreatic ascites, and pleural effusions. In these cases, endoscopic transmural drainage alone has a lower success rate, and a multimodal approach is required. The complexity of duct disruption can hinder pancreatic guidewire advancement, but pancreatic duct stenting remains the preferred treatment, as it allows downstream fluid drainage and duct healing. In this case, effective control of fluid collections was achieved through successful PD stent placement, multiple EUS-guided drainages, transmural drainage, and IR paracentesis, demonstrating the necessity of a multimodal approach in endoscopic management.
Disclosures:
Omar T. Ahmed, MD1, Kashif Osmani, MD1, Michael Gianarakis, MD1, Islam Mohamed, MD2, Ashley A. Vareedayah, MD1. P3566 - Managing Disrupted Pancreatic Duct Syndrome With a Multimodal Endoscopic Approach, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Illinois at Chicago, Chicago, IL; 2University of Missouri - Kansas City School of Medicine, Kansas City, MO
Introduction: Disrupted pancreatic duct syndrome (DrPDS) involves a partial interruption of the pancreatic duct (PD), resulting from severe necrotizing pancreatitis. It is challenging to diagnose, requiring ERCP for confirmation. This case highlights the complexities and endoscopic management strategies for DrPDS.
Case Description/Methods: A 62-year-old male with a history of alcohol use disorder and active tobacco use presented with lower extremity swelling, abdominal pain, and diarrhea. The patient was afebrile and tachycardic with a cachectic appearance and a firm, distended, and tender abdomen. Labs showed leukocytosis, mildly elevated lipase, and new AKI. CT abdomen/pelvis (CTAP) revealed acute and chronic pancreatitis with multiple large pancreatic pseudocysts compressing on the inferior vena cava and duodenum (Fig. 1).
The patient underwent endoscopic ultrasound (EUS) with placement of lumen-apposing metal stents to create cyst-duodenostomy and cyst-gastrostomy to drain two large pseudocysts, and aspirated a third large cyst. Despite initially stabilizing, the patient developed sepsis from a new, infected pseudocyst that was aspirated on repeat EUS, and cultures grew candida Krusei and tropicalis and E. facium. The patient also developed pancreatic ascites with secondary peritonitis and bilateral pleural effusions. Concerns about DrPDS prompted an ERCP, which revealed contrast extravasation in the genu and tail areas on the pancreatogram, confirming the diagnosis (Fig. 2). A pancreatic guidewire was navigated across the disrupted area in the genu, enabling the placement of a long pancreatic duct stent. CTAP two months later demonstrated near-complete resolution of pseudocysts (Fig. 3) and ERCP 8 weeks later showed no contrast extravasation on pancreatogram (Fig. 4).
Discussion: In DrPDS, persistent pancreatic fluid leakage leads to recurrent fluid collections, pseudocysts, pancreatic ascites, and pleural effusions. In these cases, endoscopic transmural drainage alone has a lower success rate, and a multimodal approach is required. The complexity of duct disruption can hinder pancreatic guidewire advancement, but pancreatic duct stenting remains the preferred treatment, as it allows downstream fluid drainage and duct healing. In this case, effective control of fluid collections was achieved through successful PD stent placement, multiple EUS-guided drainages, transmural drainage, and IR paracentesis, demonstrating the necessity of a multimodal approach in endoscopic management.
Figure: Fig. 1: CT abdomen/pelvis with multiple large pancreatic pseudocysts compressing on the inferior vena cava and duodenum.
Fig. 2: Contrast extravasation in the tail of the pancreas on the pancreatogram.
Fig. 3: CT abdomen/pelvis two months later demonstrated near-complete resolution of pseudocysts.
Fig. 4: ERCP 8 weeks later with no contrast extravasation on pancreatogram.
Fig. 2: Contrast extravasation in the tail of the pancreas on the pancreatogram.
Fig. 3: CT abdomen/pelvis two months later demonstrated near-complete resolution of pseudocysts.
Fig. 4: ERCP 8 weeks later with no contrast extravasation on pancreatogram.
Disclosures:
Omar Ahmed indicated no relevant financial relationships.
Kashif Osmani indicated no relevant financial relationships.
Michael Gianarakis indicated no relevant financial relationships.
Islam Mohamed indicated no relevant financial relationships.
Ashley Vareedayah: Boston scientific – Consultant. Conmed – Consultant.
Omar T. Ahmed, MD1, Kashif Osmani, MD1, Michael Gianarakis, MD1, Islam Mohamed, MD2, Ashley A. Vareedayah, MD1. P3566 - Managing Disrupted Pancreatic Duct Syndrome With a Multimodal Endoscopic Approach, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
