Tuesday Poster Session
Category: Biliary/Pancreas
P3580 - Cloaked Identity, Early T-Cell Precursor Lymphoblastic Leukemia (ETP-ALL) Masquerading as Autoimmune Pancreatitis
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- MN
Mahum Nadeem, MBBS
Virginia Commonwealth University Health System
Henrico, VA
Presenting Author(s)
Award: Presidential Poster Award
Mahum Nadeem, MBBS1, Shreya Garg, DO1, Dan McEntire, MD2, Bryce S. Hatfield, MD3, Ravi Vachhani, MD3
1Virginia Commonwealth University Health System, Henrico, VA; 2Virginia Commonwealth University Medical Center, Richmond, VA; 3Virginia Commonwealth University Health System, Richmond, VA
Introduction: Early precursor T cell acute lymphoblastic leukemia (ETP-ALL) is rare, affecting about three per million annually, primarily males in their teens to early twenties. The classic presentation is lymphadenopathy (LAD) or a mediastinal mass. Abdominal involvement is rare and affects the liver and spleen. We report a case of a young male with abdominal LAD and recurrent acute pancreatitis secondary to leukemic infiltration mimicking autoimmune pancreatitis.
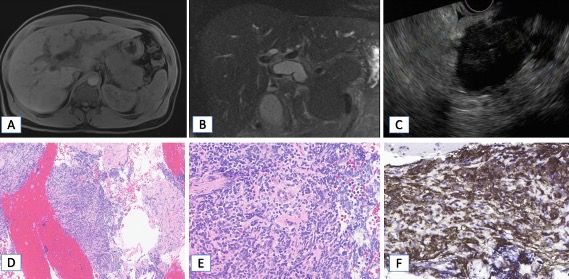
Case Description/Methods: A 35-year-old male with a history of two acute pancreatitis episodes in the past year presented with progressive abdominal pain and a 20-pound weight loss. Work-up was negative for gallstones, alcohol use, hypercalcemia, medications, or inflammatory bowel disease. Labs showed: AST 84 U/L, ALT 125 U/L, ALP 325 U/L, bilirubin 22.7 (direct 14.9) μmol/L, and normal lipase. CT revealed an enlarged pancreas with a 3.5 cm ill-defined mass in the head, causing biliary obstruction and abdominal LAD. MRI showed an edematous, sausage-shaped pancreas, suggesting autoimmune pancreatitis. He underwent ERCP and EUS with fine-needle biopsy of the pancreatic head, and placement of fully-covered metal stents (FCSEMS) in the common bile duct. Cytopathology showed benign pancreatic parenchyma with marked fibrosis and a dense lymphoplasmacytic infiltrate, predominantly lymphocytes, and few plasma cells; IgG4 staining was negative.
The patient was readmitted with worsening abdominal pain, fever, jaundice, and E. coli septicemia. Imaging raised concerns of acute cholecystitis, leading to FCSEMS exchange for plastic stents, to rule out any stent-related cystic duct occlusion. Persistent symptoms, abnormal liver enzymes, and leukocytosis resulted in a subtotal cholecystectomy and liver biopsy. Pathology revealed severe chronic cholecystitis and periportal inflammation, bile ductular proliferation, and mild steatosis. Despite negative IgG4 studies, due to high suspicion of autoimmune pancreatitis steroids were started with no improvement. Persistent leukocytosis prompted a peripheral smear and flow cytometry, revealing ETP-ALL. Based on this, a review of gallbladder, liver, and pancreas confirmed T-lymphoblastic leukemia/lymphoma infiltration in all specimens
Discussion: Acute pancreatitis is a rare presenting symptom of ETP-ALL. Despite convincing features of autoimmune pancreatitis, this case was a diagnostic challenge and underscores the importance of broad differential diagnosis especially when conventional treatments do not alleviate symptoms
Disclosures:
Mahum Nadeem, MBBS1, Shreya Garg, DO1, Dan McEntire, MD2, Bryce S. Hatfield, MD3, Ravi Vachhani, MD3. P3580 - Cloaked Identity, Early T-Cell Precursor Lymphoblastic Leukemia (ETP-ALL) Masquerading as Autoimmune Pancreatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Mahum Nadeem, MBBS1, Shreya Garg, DO1, Dan McEntire, MD2, Bryce S. Hatfield, MD3, Ravi Vachhani, MD3
1Virginia Commonwealth University Health System, Henrico, VA; 2Virginia Commonwealth University Medical Center, Richmond, VA; 3Virginia Commonwealth University Health System, Richmond, VA
Introduction: Early precursor T cell acute lymphoblastic leukemia (ETP-ALL) is rare, affecting about three per million annually, primarily males in their teens to early twenties. The classic presentation is lymphadenopathy (LAD) or a mediastinal mass. Abdominal involvement is rare and affects the liver and spleen. We report a case of a young male with abdominal LAD and recurrent acute pancreatitis secondary to leukemic infiltration mimicking autoimmune pancreatitis.
Case Description/Methods: A 35-year-old male with a history of two acute pancreatitis episodes in the past year presented with progressive abdominal pain and a 20-pound weight loss. Work-up was negative for gallstones, alcohol use, hypercalcemia, medications, or inflammatory bowel disease. Labs showed: AST 84 U/L, ALT 125 U/L, ALP 325 U/L, bilirubin 22.7 (direct 14.9) μmol/L, and normal lipase. CT revealed an enlarged pancreas with a 3.5 cm ill-defined mass in the head, causing biliary obstruction and abdominal LAD. MRI showed an edematous, sausage-shaped pancreas, suggesting autoimmune pancreatitis. He underwent ERCP and EUS with fine-needle biopsy of the pancreatic head, and placement of fully-covered metal stents (FCSEMS) in the common bile duct. Cytopathology showed benign pancreatic parenchyma with marked fibrosis and a dense lymphoplasmacytic infiltrate, predominantly lymphocytes, and few plasma cells; IgG4 staining was negative.
The patient was readmitted with worsening abdominal pain, fever, jaundice, and E. coli septicemia. Imaging raised concerns of acute cholecystitis, leading to FCSEMS exchange for plastic stents, to rule out any stent-related cystic duct occlusion. Persistent symptoms, abnormal liver enzymes, and leukocytosis resulted in a subtotal cholecystectomy and liver biopsy. Pathology revealed severe chronic cholecystitis and periportal inflammation, bile ductular proliferation, and mild steatosis. Despite negative IgG4 studies, due to high suspicion of autoimmune pancreatitis steroids were started with no improvement. Persistent leukocytosis prompted a peripheral smear and flow cytometry, revealing ETP-ALL. Based on this, a review of gallbladder, liver, and pancreas confirmed T-lymphoblastic leukemia/lymphoma infiltration in all specimens
Discussion: Acute pancreatitis is a rare presenting symptom of ETP-ALL. Despite convincing features of autoimmune pancreatitis, this case was a diagnostic challenge and underscores the importance of broad differential diagnosis especially when conventional treatments do not alleviate symptoms
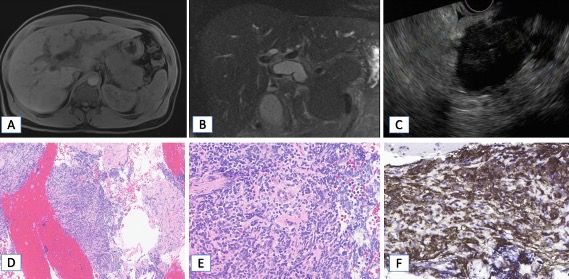
Figure: A,B: MRI/MRCP images showing diffuse loss of intrinsic T1 hyperintensity throughout the pancreas with subtle rim of relative T1 hyperintensity (A). Pancreas is diffusely edematous and sausage-shaped with a subtle T2 hypointense rim (B). There is diffuse restricted diffusion throughout the pancreas
C: EUS showing diffuse hypoechoic parenchyma in the body of the pancreas
D: Low power (100x HE) showing a dense mononuclear cell infiltrate
E: 400x HE. Neoplastic cells with scant cytoplasm, delicate chromatin, and indistinct nucleoli.
F: 400x CD3 positive – T cell marker
C: EUS showing diffuse hypoechoic parenchyma in the body of the pancreas
D: Low power (100x HE) showing a dense mononuclear cell infiltrate
E: 400x HE. Neoplastic cells with scant cytoplasm, delicate chromatin, and indistinct nucleoli.
F: 400x CD3 positive – T cell marker
Disclosures:
Mahum Nadeem indicated no relevant financial relationships.
Shreya Garg indicated no relevant financial relationships.
Dan McEntire indicated no relevant financial relationships.
Bryce Hatfield indicated no relevant financial relationships.
Ravi Vachhani indicated no relevant financial relationships.
Mahum Nadeem, MBBS1, Shreya Garg, DO1, Dan McEntire, MD2, Bryce S. Hatfield, MD3, Ravi Vachhani, MD3. P3580 - Cloaked Identity, Early T-Cell Precursor Lymphoblastic Leukemia (ETP-ALL) Masquerading as Autoimmune Pancreatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

