Tuesday Poster Session
Category: Colon
P3626 - Precutting Endoscopic Mucosal Resection Compared to Conventional Endoscopic Mucosal Resection and Endoscopic Submucosal Dissection for Colorectal Neoplasia: A Systematic Review and Meta-Analysis
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Azizullah Beran, MD
Indiana University School of Medicine
Indianapolis, IN
Presenting Author(s)
Azizullah Beran, MD1, Tarek G. Aridi, MD1, Mohammad Bilal, MD2, John M. DeWitt, MD, FACG1, Mohammad Al-Haddad, MD, FACG1, John Guardiola, MD1
1Indiana University School of Medicine, Indianapolis, IN; 2University of Minnesota and Minneapolis VA Health Care System, Minneapolis, MN
Introduction: Endoscopic submucosal dissection (ESD) is superior to piecemeal endoscopic mucosal resection (PM-EMR) for curative resection of colorectal neoplasia but involves longer procedures and higher risks and costs. Precutting EMR (PC-EMR), which involves a circumferential incision before mucosal resection, may improve curative resection rates over PM-EMR with lower risks and costs than ESD.
Methods: We searched PubMed, Embase, and Web of Science databases through February 2024 for all studies that compared the outcomes of PC-EMR with PM-EMR and/or ESD for colorectal neoplasia. Pooled risk ratios (RR) and mean differences (MD) with 95% confidence intervals (CIs) were obtained using a random-effect model. The primary outcomes were en-bloc resection and complete resection rates. Complete resection was defined as en-bloc resection with negative histological negative margins. Secondary outcomes were procedure time, bleeding, and perforation rates.
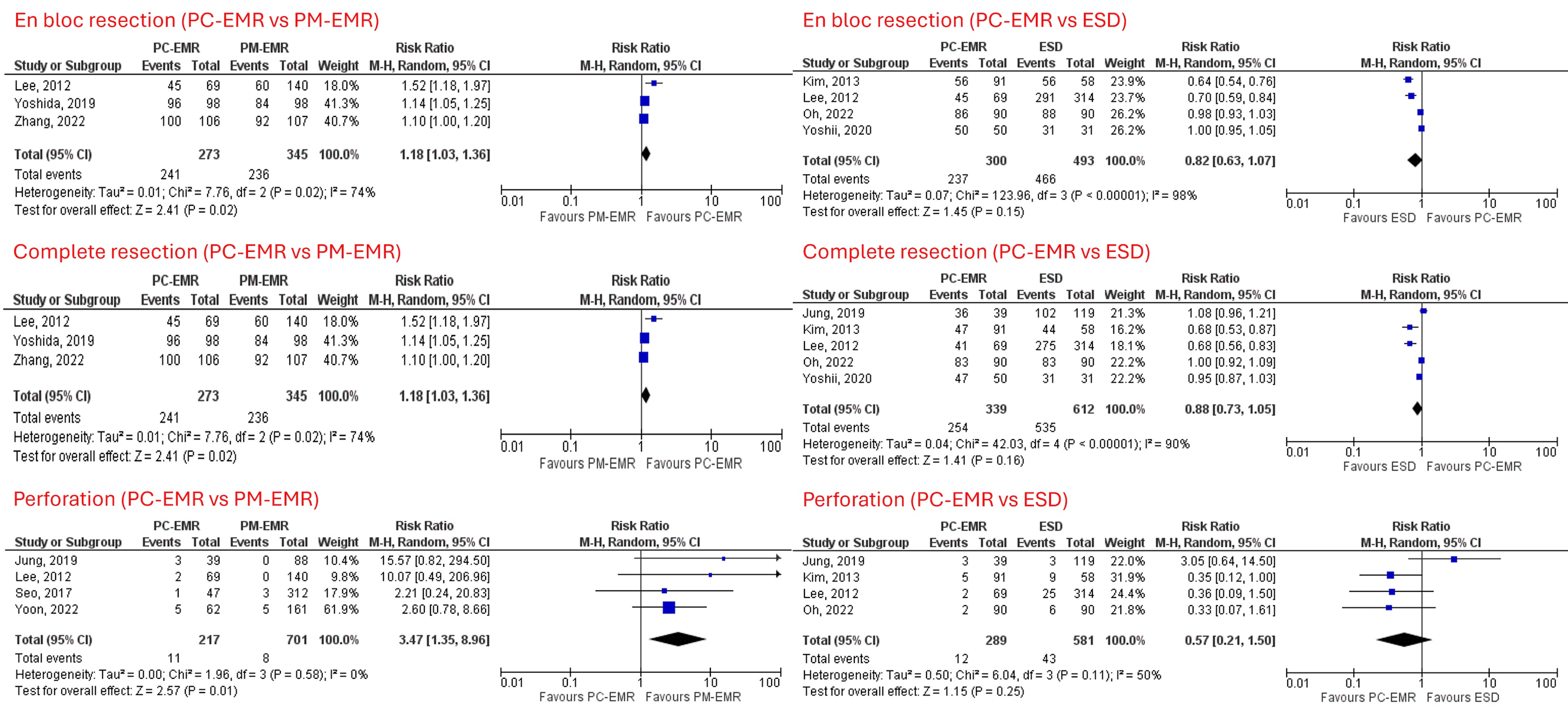
Results: Out of 223 studies screened, nine studies with 2,136 patients and 2,170 neoplastic lesions (PC-EMR=652, PM-EMR= 906, and ESD=612) were included. Of 2,170 neoplastic lesions, 76% were adenomas. Compared to PM-EMR, PC-EMR was associated with higher en-bloc resection (RR 1.18, 95% CI 1.03-1.36, P=0.02, I2=74%, Figure 1) and complete resection (RR 1.17, CI 1.01-1.37, P=0.04, I2=68%, Figure 1), but had higher perforation (RR 3.47, CI 1.35-8.96, P=0.01, I2=0%, Figure 1) and longer procedure time (MD 11.63 minutes; CI 5.73, 17.54; P< 0.001, I2=97%) and similar bleeding risks (RR 1.23, CI 0.51-2.98, P=0.64, I2=61%). Compared to ESD, PC-EMR had comparable en-bloc resection (RR 0.82, CI 0.63-1.07, P=0.15, I2=98%, Figure 1), complete resection (RR 0.88, CI 0.73-1.05, P=0.16, I2=90%, Figure 1), bleeding (RR 2.13, CI 0.48-9.51, P=0.32, I2=16%), perforation (RR 0.57, CI 0.21-1.50, P=0.25, I2=50%, Figure 1), but had shorter procedure times (MD -25.21 minutes; CI -33.32, -17.10; P< 0.001, I2=84%).
Discussion: PC-EMR was associated with higher en-bloc and complete resection than PM-EMR but at the cost of higher perforation rates and longer procedure times, but similar bleeding rates. PC-EMR was non-inferior to ESD in en-bloc and complete resections, had shorter procedure times and comparable bleeding and perforation rates to ESD. PC-EMR may be a promising technique that bridges PM-EMR and ESD for the resection of colorectal neoplasia. Further RCTs are needed to validate our findings.
Disclosures:
Azizullah Beran, MD1, Tarek G. Aridi, MD1, Mohammad Bilal, MD2, John M. DeWitt, MD, FACG1, Mohammad Al-Haddad, MD, FACG1, John Guardiola, MD1. P3626 - Precutting Endoscopic Mucosal Resection Compared to Conventional Endoscopic Mucosal Resection and Endoscopic Submucosal Dissection for Colorectal Neoplasia: A Systematic Review and Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Indiana University School of Medicine, Indianapolis, IN; 2University of Minnesota and Minneapolis VA Health Care System, Minneapolis, MN
Introduction: Endoscopic submucosal dissection (ESD) is superior to piecemeal endoscopic mucosal resection (PM-EMR) for curative resection of colorectal neoplasia but involves longer procedures and higher risks and costs. Precutting EMR (PC-EMR), which involves a circumferential incision before mucosal resection, may improve curative resection rates over PM-EMR with lower risks and costs than ESD.
Methods: We searched PubMed, Embase, and Web of Science databases through February 2024 for all studies that compared the outcomes of PC-EMR with PM-EMR and/or ESD for colorectal neoplasia. Pooled risk ratios (RR) and mean differences (MD) with 95% confidence intervals (CIs) were obtained using a random-effect model. The primary outcomes were en-bloc resection and complete resection rates. Complete resection was defined as en-bloc resection with negative histological negative margins. Secondary outcomes were procedure time, bleeding, and perforation rates.
Results: Out of 223 studies screened, nine studies with 2,136 patients and 2,170 neoplastic lesions (PC-EMR=652, PM-EMR= 906, and ESD=612) were included. Of 2,170 neoplastic lesions, 76% were adenomas. Compared to PM-EMR, PC-EMR was associated with higher en-bloc resection (RR 1.18, 95% CI 1.03-1.36, P=0.02, I2=74%, Figure 1) and complete resection (RR 1.17, CI 1.01-1.37, P=0.04, I2=68%, Figure 1), but had higher perforation (RR 3.47, CI 1.35-8.96, P=0.01, I2=0%, Figure 1) and longer procedure time (MD 11.63 minutes; CI 5.73, 17.54; P< 0.001, I2=97%) and similar bleeding risks (RR 1.23, CI 0.51-2.98, P=0.64, I2=61%). Compared to ESD, PC-EMR had comparable en-bloc resection (RR 0.82, CI 0.63-1.07, P=0.15, I2=98%, Figure 1), complete resection (RR 0.88, CI 0.73-1.05, P=0.16, I2=90%, Figure 1), bleeding (RR 2.13, CI 0.48-9.51, P=0.32, I2=16%), perforation (RR 0.57, CI 0.21-1.50, P=0.25, I2=50%, Figure 1), but had shorter procedure times (MD -25.21 minutes; CI -33.32, -17.10; P< 0.001, I2=84%).
Discussion: PC-EMR was associated with higher en-bloc and complete resection than PM-EMR but at the cost of higher perforation rates and longer procedure times, but similar bleeding rates. PC-EMR was non-inferior to ESD in en-bloc and complete resections, had shorter procedure times and comparable bleeding and perforation rates to ESD. PC-EMR may be a promising technique that bridges PM-EMR and ESD for the resection of colorectal neoplasia. Further RCTs are needed to validate our findings.
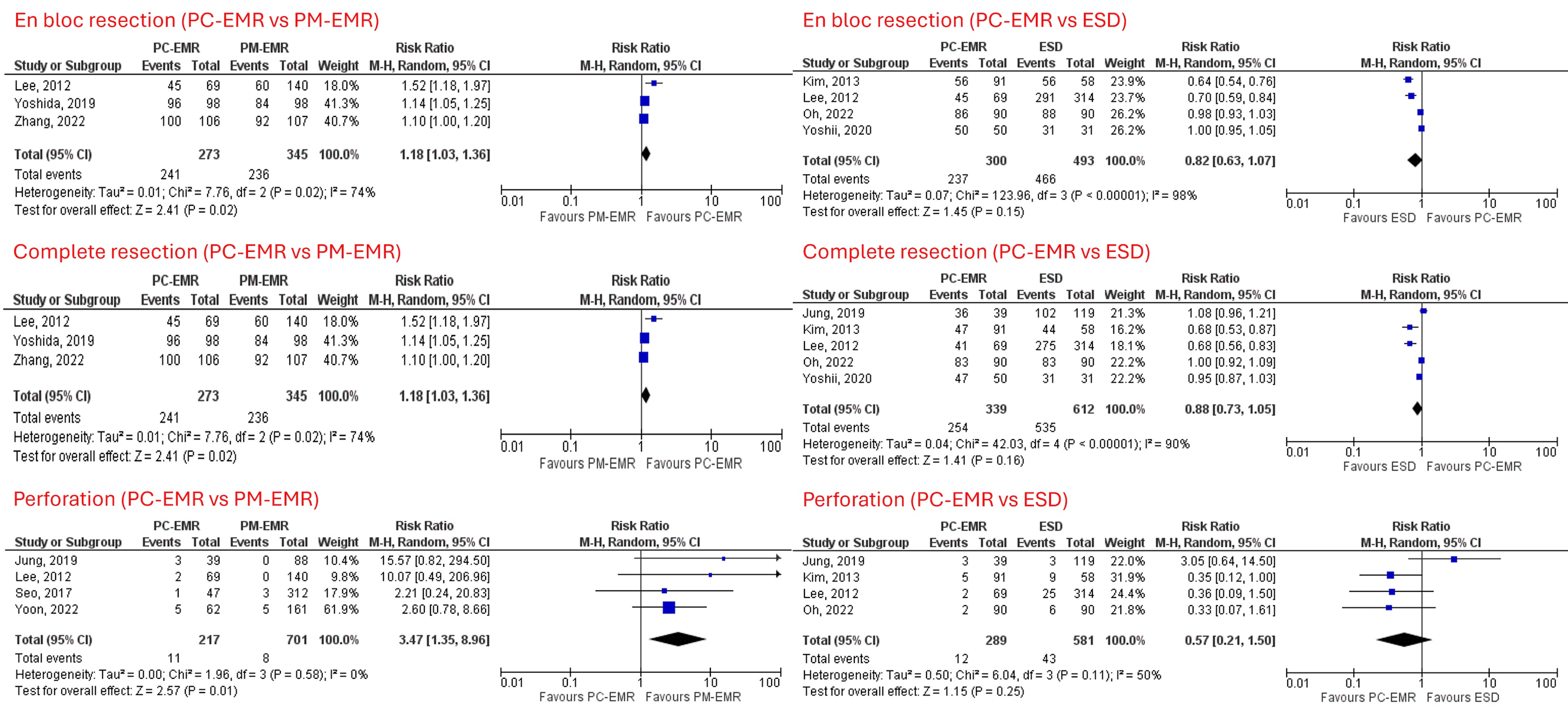
Figure: Compared to PM-EMR, PC-EMR was associated with higher en-bloc resection and complete resection but had higher perforation and longer procedure time and similar bleeding risks. Compared to ESD, PC-EMR had comparable en-bloc resection and complete resection, bleeding and perforation risks, but had shorter procedure times.
Disclosures:
Azizullah Beran indicated no relevant financial relationships.
Tarek Aridi indicated no relevant financial relationships.
Mohammad Bilal: Boston Scientific – Consultant. Cook endoscopy – Speakers Bureau.
John DeWitt indicated no relevant financial relationships.
Mohammad Al-Haddad: Amplified Sciences – Grant/Research Support. Boston Scientific – Consultant. Interpace Diagnostics – Consultant.
John Guardiola: Boston Scientific Corporation – Travel Support. Olympus Corporation – Travel Support.
Azizullah Beran, MD1, Tarek G. Aridi, MD1, Mohammad Bilal, MD2, John M. DeWitt, MD, FACG1, Mohammad Al-Haddad, MD, FACG1, John Guardiola, MD1. P3626 - Precutting Endoscopic Mucosal Resection Compared to Conventional Endoscopic Mucosal Resection and Endoscopic Submucosal Dissection for Colorectal Neoplasia: A Systematic Review and Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
