Tuesday Poster Session
Category: Colon
P3686 - Incidental Finding of Mucosa-Associated Lymphoid Tissue Lymphoma on Screening Colonoscopy
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- RP
Rakhi Patel, DO
Arizona College of Osteopathic Medicine, Midwestern University
Las Vegas, NV
Presenting Author(s)
Rakhi Patel, DO1, Jennifer Raffel, MD2, Hussein Al-Hamid, MD3
1Arizona College of Osteopathic Medicine, Midwestern University, Las Vegas, NV; 2P4 Diagnostix Clinical Pathology Network, Tempe, AZ; 3HonorHealth, Scottsdale, AZ
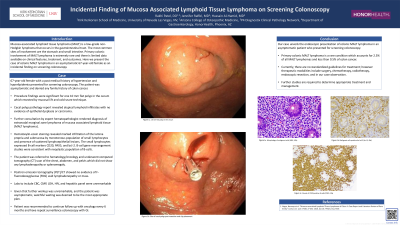
Introduction: Mucosa-associated lymphoid tissue (MALT) lymphoma is a low-grade non-Hodgkin lymphoma that occurs in the gastrointestinal tract. The most common sites of involvement are the stomach and small intestine. Primary colonic involvement of MALT lymphoma is extremely rare and there is limited data on clinical features, treatment, and outcomes. We present the case of colonic MALT lymphoma in a 67-year-old female as an incidental finding on screening colonoscopy.
Case Description/Methods: A 67-year-old female with a past medical history of hypertension and hyperlipidemia presented for screening colonoscopy. The patient was asymptomatic and denied any family history of colon cancer. Procedure findings were significant for one 10 mm flat polyp in the cecum which resected by mucosal lift and cold snare technique. Pathology report revealed atypical lymphoid infiltrates with no evidence of epithelial dysplasia or carcinoma. Further consultation by expert hematopathologist rendered diagnosis of extranodal marginal zone MALT lymphoma. Hematoxylin-eosin staining revealed marked infiltration of the lamina propria and submucosa by monotonous population of small lymphocytes and presence of scattered lymphoepithelial lesions. The small lymphocytes expressed B-cell markers CD20, PAX5, and bcl-2. B-cell gene rearrangement studies were consistent with neoplastic population of B-cells. The patient was referred to oncology and underwent computed tomography (CT) scan of the chest, abdomen, and pelvis which did not show any lymphadenopathy or splenomegaly. Positron emission tomography (PET)/CT showed no evidence of F-fluorodeoxyglucose (FDG) avid lymphadenopathy or mass. Labs to include CBC, CMP, LDH, HIV, and hepatitis panel were unremarkable. Given that further workup was unremarkable, and the patient was asymptomatic, watchful waiting was deemed to be the most appropriate plan. Patient was recommended to continue follow up with oncology every 6 months and have repeat surveillance colonoscopy with GI.
Discussion: This case highlights the endoscopic presentation of colonic MALT lymphoma in an asymptomatic patient who presented for screening colonoscopy. Primary colonic presentation is rare, accounting for 2.5% of all MALT lymphomas and less than 0.5% of colon cancer. Currently, there are no standardized guidelines for treatment; however therapeutic modalities include surgery, chemotherapy, radiotherapy, endoscopic resection, or observation. Further studies are required to determine appropriate treatment and management.
Disclosures:
Rakhi Patel, DO1, Jennifer Raffel, MD2, Hussein Al-Hamid, MD3. P3686 - Incidental Finding of Mucosa-Associated Lymphoid Tissue Lymphoma on Screening Colonoscopy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Arizona College of Osteopathic Medicine, Midwestern University, Las Vegas, NV; 2P4 Diagnostix Clinical Pathology Network, Tempe, AZ; 3HonorHealth, Scottsdale, AZ
Introduction: Mucosa-associated lymphoid tissue (MALT) lymphoma is a low-grade non-Hodgkin lymphoma that occurs in the gastrointestinal tract. The most common sites of involvement are the stomach and small intestine. Primary colonic involvement of MALT lymphoma is extremely rare and there is limited data on clinical features, treatment, and outcomes. We present the case of colonic MALT lymphoma in a 67-year-old female as an incidental finding on screening colonoscopy.
Case Description/Methods: A 67-year-old female with a past medical history of hypertension and hyperlipidemia presented for screening colonoscopy. The patient was asymptomatic and denied any family history of colon cancer. Procedure findings were significant for one 10 mm flat polyp in the cecum which resected by mucosal lift and cold snare technique. Pathology report revealed atypical lymphoid infiltrates with no evidence of epithelial dysplasia or carcinoma. Further consultation by expert hematopathologist rendered diagnosis of extranodal marginal zone MALT lymphoma. Hematoxylin-eosin staining revealed marked infiltration of the lamina propria and submucosa by monotonous population of small lymphocytes and presence of scattered lymphoepithelial lesions. The small lymphocytes expressed B-cell markers CD20, PAX5, and bcl-2. B-cell gene rearrangement studies were consistent with neoplastic population of B-cells. The patient was referred to oncology and underwent computed tomography (CT) scan of the chest, abdomen, and pelvis which did not show any lymphadenopathy or splenomegaly. Positron emission tomography (PET)/CT showed no evidence of F-fluorodeoxyglucose (FDG) avid lymphadenopathy or mass. Labs to include CBC, CMP, LDH, HIV, and hepatitis panel were unremarkable. Given that further workup was unremarkable, and the patient was asymptomatic, watchful waiting was deemed to be the most appropriate plan. Patient was recommended to continue follow up with oncology every 6 months and have repeat surveillance colonoscopy with GI.
Discussion: This case highlights the endoscopic presentation of colonic MALT lymphoma in an asymptomatic patient who presented for screening colonoscopy. Primary colonic presentation is rare, accounting for 2.5% of all MALT lymphomas and less than 0.5% of colon cancer. Currently, there are no standardized guidelines for treatment; however therapeutic modalities include surgery, chemotherapy, radiotherapy, endoscopic resection, or observation. Further studies are required to determine appropriate treatment and management.
Disclosures:
Rakhi Patel indicated no relevant financial relationships.
Jennifer Raffel indicated no relevant financial relationships.
Hussein Al-Hamid indicated no relevant financial relationships.
Rakhi Patel, DO1, Jennifer Raffel, MD2, Hussein Al-Hamid, MD3. P3686 - Incidental Finding of Mucosa-Associated Lymphoid Tissue Lymphoma on Screening Colonoscopy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
