Tuesday Poster Session
Category: Colon
P3690 - A Unique Cause of Colitis in a Patient with Human Immunodeficiency Virus
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- NM
Nitish Mittal, MD
University of Texas Health, McGovern Medical School
Houston, TX
Presenting Author(s)
Nitish Mittal, MD1, Antonio Pizuorno Machado, MD, MPH2, Rohan Ahuja, MD1, Faisal Ali, MD1, Suhair Al Salihi, MD1, Tanima Jana, MD, FACG1
1University of Texas Health, McGovern Medical School, Houston, TX; 2UT Southwstern Medical Center, Dallas, TX
Introduction: Patients with HIV (human immunodeficiency virus) are a unique patient population in that their immunocompromised state predisposes them to a variety of infectious conditions. Colitis in HIV patients are commonly related to bacterial, viral, or fungal conditions. A lesser-known cause of colitis in an HIV patient is sexually transmitted infections. Herein, we present the case of a 36-year-old man with HIV who presented with hematochezia and severe weight loss and was ultimately diagnosed with syphilitic colitis.
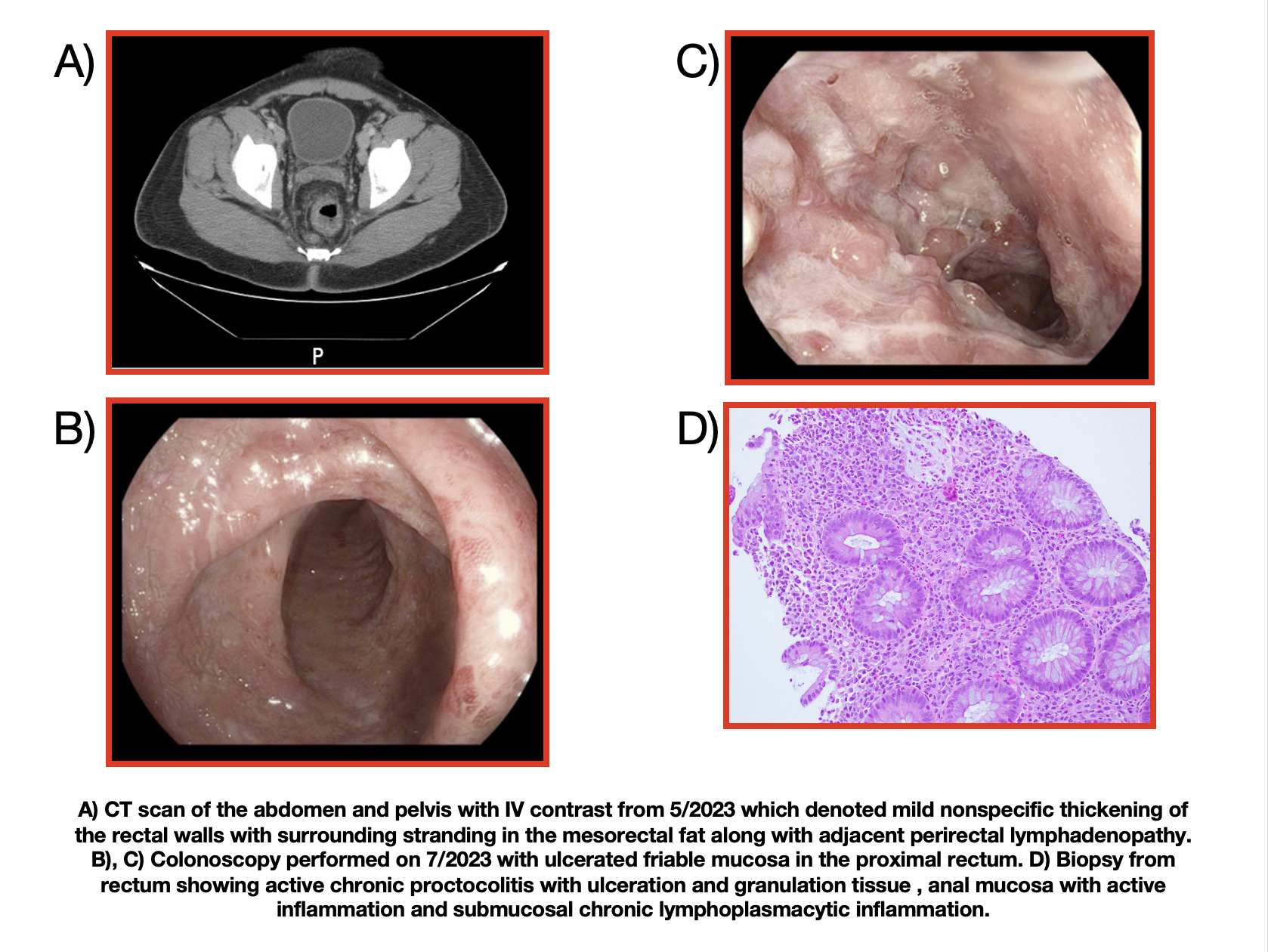
Case Description/Methods: A 36-year-old African American man with a history of HIV/acquired immunodeficiency syndrome (AIDS), non-compliant with bictegravir, emtricitabine and tenofovir alafenamide, presented to clinic with hematochezia and unintentional 40-pound weight loss over the past year. CT scan of the abdomen and pelvis showed non-specific mid to distal rectal wall thickening (Figure 1A) with surrounding perirectal lymphadenopathy. He underwent upper endoscopy/colonoscopy with findings of gastric erythema, polypoidal lesions in the rectosigmoid region, and ulcerated mucosa in the rectum (Figure 1B and 1C). Biopsies showed helicobacter pylori gastritis and active chronic proctocolitis (Figure 1D). Cytomegalovirus (CMV) and herpes simplex virus (HSV) stains were negative, and a spirochete immunohistochemical stain showed nonspecific binding. The patient’s prior history was then examined further, and it was noted that he had been treated in the past for latent syphilis. New labs showed positive treponema pallidum particle agglutination (TP-PA) antibodies and an elevated rapid plasma regain (RPR) titer of 1:1 (was previously 1:4). He was treated with bismuth quadruple therapy, a one-time dose of ceftriaxone, and seven days of doxycycline (Image 2). He showed significant clinical improvement at his three-month follow-up, with appropriate weight gain and resolution of hematochezia.
Discussion: Colitis in HIV patients can be a diagnostic dilemma due to the possibility of numerous medical conditions that can mimic each other. In our patient, the pathology finding of active chronic proctocolitis suggested an infectious or inflammatory colitis, CMV, and HSV stains were negative. While inflammatory bowel disease was considered, it was further review of the patient’s history that ultimately led to a diagnosis of syphilitic colitis. The patient responded well to appropriate therapy. Our case highlights the importance of keeping a broad differential in patients with HIV infection.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Nitish Mittal, MD1, Antonio Pizuorno Machado, MD, MPH2, Rohan Ahuja, MD1, Faisal Ali, MD1, Suhair Al Salihi, MD1, Tanima Jana, MD, FACG1. P3690 - A Unique Cause of Colitis in a Patient with Human Immunodeficiency Virus, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Texas Health, McGovern Medical School, Houston, TX; 2UT Southwstern Medical Center, Dallas, TX
Introduction: Patients with HIV (human immunodeficiency virus) are a unique patient population in that their immunocompromised state predisposes them to a variety of infectious conditions. Colitis in HIV patients are commonly related to bacterial, viral, or fungal conditions. A lesser-known cause of colitis in an HIV patient is sexually transmitted infections. Herein, we present the case of a 36-year-old man with HIV who presented with hematochezia and severe weight loss and was ultimately diagnosed with syphilitic colitis.
Case Description/Methods: A 36-year-old African American man with a history of HIV/acquired immunodeficiency syndrome (AIDS), non-compliant with bictegravir, emtricitabine and tenofovir alafenamide, presented to clinic with hematochezia and unintentional 40-pound weight loss over the past year. CT scan of the abdomen and pelvis showed non-specific mid to distal rectal wall thickening (Figure 1A) with surrounding perirectal lymphadenopathy. He underwent upper endoscopy/colonoscopy with findings of gastric erythema, polypoidal lesions in the rectosigmoid region, and ulcerated mucosa in the rectum (Figure 1B and 1C). Biopsies showed helicobacter pylori gastritis and active chronic proctocolitis (Figure 1D). Cytomegalovirus (CMV) and herpes simplex virus (HSV) stains were negative, and a spirochete immunohistochemical stain showed nonspecific binding. The patient’s prior history was then examined further, and it was noted that he had been treated in the past for latent syphilis. New labs showed positive treponema pallidum particle agglutination (TP-PA) antibodies and an elevated rapid plasma regain (RPR) titer of 1:1 (was previously 1:4). He was treated with bismuth quadruple therapy, a one-time dose of ceftriaxone, and seven days of doxycycline (Image 2). He showed significant clinical improvement at his three-month follow-up, with appropriate weight gain and resolution of hematochezia.
Discussion: Colitis in HIV patients can be a diagnostic dilemma due to the possibility of numerous medical conditions that can mimic each other. In our patient, the pathology finding of active chronic proctocolitis suggested an infectious or inflammatory colitis, CMV, and HSV stains were negative. While inflammatory bowel disease was considered, it was further review of the patient’s history that ultimately led to a diagnosis of syphilitic colitis. The patient responded well to appropriate therapy. Our case highlights the importance of keeping a broad differential in patients with HIV infection.
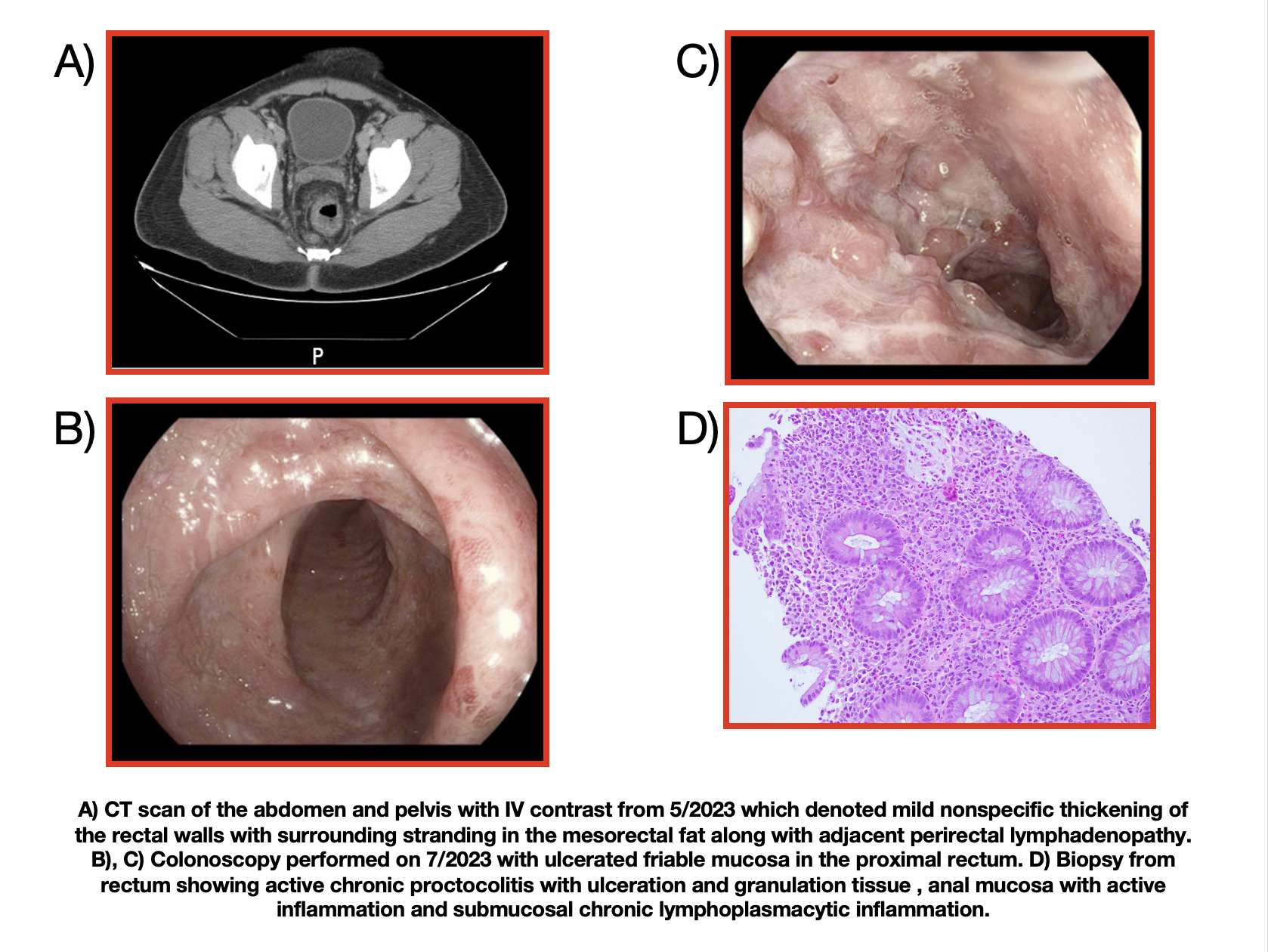
Figure: CT a/p (Figure 1A), colonoscopy (Figure 1B and 1C), pathology (Figure 1D)
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Nitish Mittal indicated no relevant financial relationships.
Antonio Pizuorno Machado indicated no relevant financial relationships.
Rohan Ahuja indicated no relevant financial relationships.
Faisal Ali indicated no relevant financial relationships.
Suhair Al Salihi indicated no relevant financial relationships.
Tanima Jana indicated no relevant financial relationships.
Nitish Mittal, MD1, Antonio Pizuorno Machado, MD, MPH2, Rohan Ahuja, MD1, Faisal Ali, MD1, Suhair Al Salihi, MD1, Tanima Jana, MD, FACG1. P3690 - A Unique Cause of Colitis in a Patient with Human Immunodeficiency Virus, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
