Tuesday Poster Session
Category: Colon
P3705 - Colonic Tuberculosis: A Case Report and Literature Review of the Endoscopic, Radiographic, and Biopsy Findings
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Essam Rashad, MBBCh
Parkview Medical Center
Fort Wayne, IN
Presenting Author(s)
Essam Rashad, MBBCh1, Ranran Zhang, MD, PhD2, Jad El Bulbul, MD3
1Parkview Medical Center, Fort Wayne, IN; 2Parkview Reginal Medical Center, Fort Wayne, IN; 3University of Arizona, Tucson, AZ
Introduction: Tuberculosis (TB) primarily affects the lungs, but extrapulmonary manifestations such as colonic TB, though rare, can occur. Colonic TB can mimic inflammatory bowel disease (IBD), presenting a diagnostic challenge due to overlapping symptoms. This case highlights the importance of considering TB in the differential diagnosis of chronic gastrointestinal symptoms, especially in patients from TB-endemic regions.
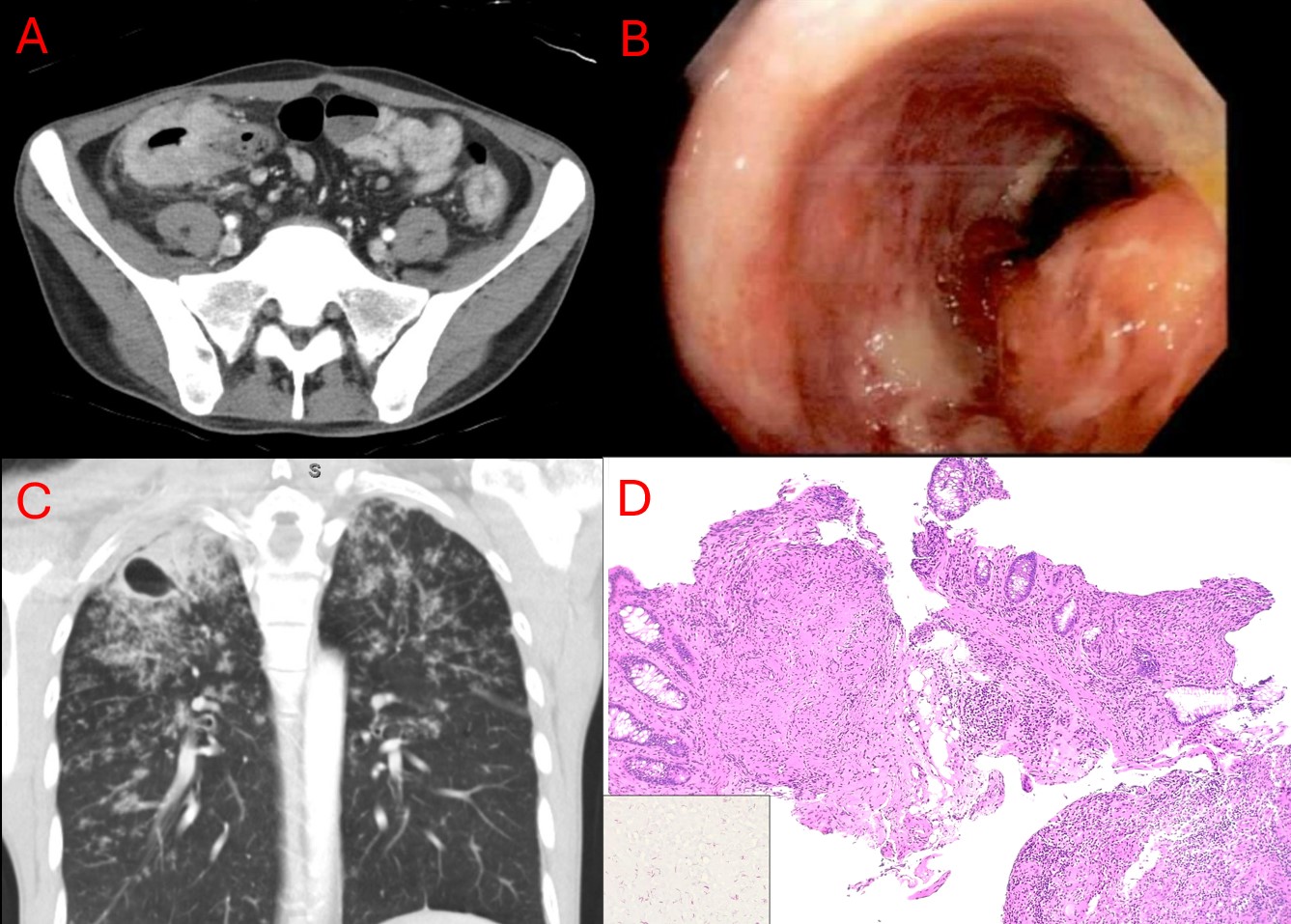
Case Description/Methods: A 36-year-old male presented with a 1-year history of intermittent abdominal pain, diarrhea, night sweats, fatigue, and melenic stools that worsened over the past two months, resulting in a 30-pound weight loss. Initial examination revealed a BMI of 18 kg/m² and abdominal tenderness in the right lower quadrant. CT imaging revealed severe circumferential wall thickening of the ascending colon with inflammatory stranding and mesenteric lymphadenopathy. A lymph node biopsy revealed necrotizing granulomas negative for malignancy and acid-fast bacilli (AFB) stain. During a second admission, persistent abdominal pain and bloody stools led to a colonoscopy, which showed scattered inflammation and a polypoid tumor at the splenic flexure, leading to a diagnosis of IBD. Biopsies later revealed necrotizing granulomatous inflammation with AFB-positive mycobacterial organisms, mimicking chronic active colitis. CT chest revealed a cavitary lesion in the right lung apex, consistent with reactivation tuberculosis. Sputum samples were positive for AFB, confirming the diagnosis. The patient was started on RIPE therapy (rifampin, INH, pyrazinamide, ethambutol).
Discussion: Gastrointestinal TB accounts for 1-3% of all TB cases. Colonic TB can closely resemble IBD, particularly Crohn's disease. Typical endoscopic findings include ulcers with irregular margins, nodules, pseudopolyps, and strictures. Radiographic studies often show bowel wall thickening and lymphadenopathy, while biopsy findings commonly reveal granulomatous inflammation with caseation and AFB-positive organisms. In this case, the patient's symptoms and initial diagnostic findings suggested Crohn's disease, but biopsy results confirming necrotizing granulomas and AFB-positive organisms (identified only on the second biopsy) ultimately led to the correct diagnosis of TB. This case not only underscores the importance of considering TB in the differential diagnosis, especially in endemic regions or in patients with a history of possible exposure, but also highlights the difficulty in diagnosis and known pitfalls.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Essam Rashad, MBBCh1, Ranran Zhang, MD, PhD2, Jad El Bulbul, MD3. P3705 - Colonic Tuberculosis: A Case Report and Literature Review of the Endoscopic, Radiographic, and Biopsy Findings, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Parkview Medical Center, Fort Wayne, IN; 2Parkview Reginal Medical Center, Fort Wayne, IN; 3University of Arizona, Tucson, AZ
Introduction: Tuberculosis (TB) primarily affects the lungs, but extrapulmonary manifestations such as colonic TB, though rare, can occur. Colonic TB can mimic inflammatory bowel disease (IBD), presenting a diagnostic challenge due to overlapping symptoms. This case highlights the importance of considering TB in the differential diagnosis of chronic gastrointestinal symptoms, especially in patients from TB-endemic regions.
Case Description/Methods: A 36-year-old male presented with a 1-year history of intermittent abdominal pain, diarrhea, night sweats, fatigue, and melenic stools that worsened over the past two months, resulting in a 30-pound weight loss. Initial examination revealed a BMI of 18 kg/m² and abdominal tenderness in the right lower quadrant. CT imaging revealed severe circumferential wall thickening of the ascending colon with inflammatory stranding and mesenteric lymphadenopathy. A lymph node biopsy revealed necrotizing granulomas negative for malignancy and acid-fast bacilli (AFB) stain. During a second admission, persistent abdominal pain and bloody stools led to a colonoscopy, which showed scattered inflammation and a polypoid tumor at the splenic flexure, leading to a diagnosis of IBD. Biopsies later revealed necrotizing granulomatous inflammation with AFB-positive mycobacterial organisms, mimicking chronic active colitis. CT chest revealed a cavitary lesion in the right lung apex, consistent with reactivation tuberculosis. Sputum samples were positive for AFB, confirming the diagnosis. The patient was started on RIPE therapy (rifampin, INH, pyrazinamide, ethambutol).
Discussion: Gastrointestinal TB accounts for 1-3% of all TB cases. Colonic TB can closely resemble IBD, particularly Crohn's disease. Typical endoscopic findings include ulcers with irregular margins, nodules, pseudopolyps, and strictures. Radiographic studies often show bowel wall thickening and lymphadenopathy, while biopsy findings commonly reveal granulomatous inflammation with caseation and AFB-positive organisms. In this case, the patient's symptoms and initial diagnostic findings suggested Crohn's disease, but biopsy results confirming necrotizing granulomas and AFB-positive organisms (identified only on the second biopsy) ultimately led to the correct diagnosis of TB. This case not only underscores the importance of considering TB in the differential diagnosis, especially in endemic regions or in patients with a history of possible exposure, but also highlights the difficulty in diagnosis and known pitfalls.
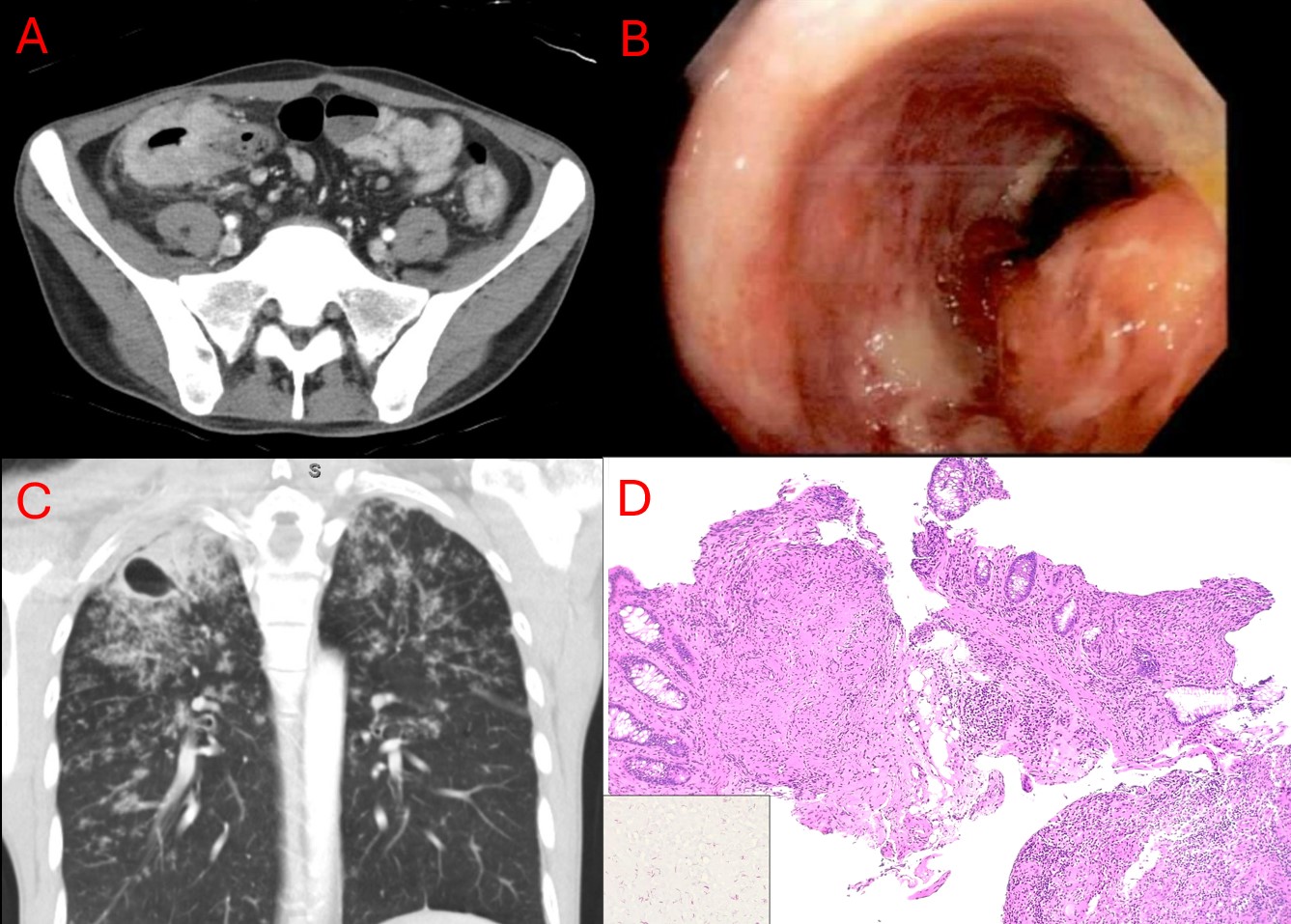
Figure: A: Severe circumferential wall thickening of the ascending colon, pericolic fat stranding and mesenteric lymphadenopathy. B: Scattered inflammation with mucus and a polypoid tumor at the splenic flexure. C: Right upper lobe cavitation. D: H&E image at 10x power with colon view at the background; AFB-positive staining seen at lower left side.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Essam Rashad indicated no relevant financial relationships.
Ranran Zhang indicated no relevant financial relationships.
Jad El Bulbul indicated no relevant financial relationships.
Essam Rashad, MBBCh1, Ranran Zhang, MD, PhD2, Jad El Bulbul, MD3. P3705 - Colonic Tuberculosis: A Case Report and Literature Review of the Endoscopic, Radiographic, and Biopsy Findings, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
