Tuesday Poster Session
Category: Colon
P3741 - Hiding in Plain Sight: Colonic Tuberculosis Mimicking Crohn’s Disease
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
Max L. Goldman, MD
Kaiser Permanente
San Francisco, CA
Presenting Author(s)
Max L. Goldman, MD, Brenton G. Davis, MD, Lyle Shlager, MD
Kaiser Permanente, San Francisco, CA
Introduction: Colonic tuberculosis (TB) is rare in immunocompetent patients, and diagnosis is often delayed due to its similar appearance on endoscopy and pathology relative to more common diseases. We present a case of colonic TB masquerading as Crohn’s disease.
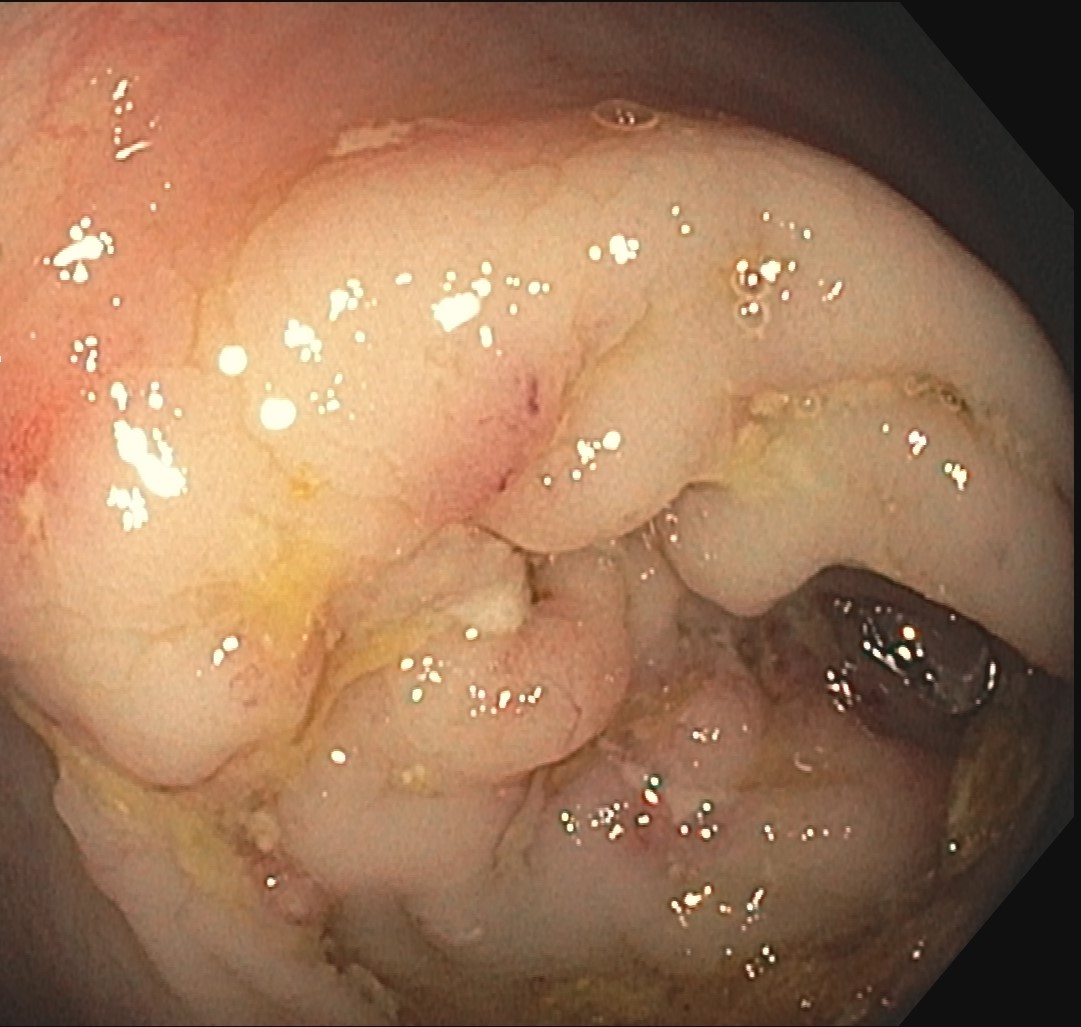
Case Description/Methods: A healthy 73-year-old man from Southeast Asia presented with a week of abdominal pain, diarrhea, and decreased appetite without fever or leukocytosis. A CT abdomen revealed cecal mural thickening and enhancement. He was discharged on empiric antibiotic treatment for diverticulitis. He represented 2 weeks later with similar symptoms and unchanged CT findings. An expedited colonoscopy was notable for an ulcerated cecal tip and ascending colonic skip lesions and nodularity. Pathology revealed chronic active colitis with ulcers and granulomas. All stains were negative for microorganisms. Ferritin was 500ng/mL, CRP 6.5mg/dL, and QuantiFERON-TB negative. The patient returned to the hospital with signs of peritonism. A repeat CT revealed a cecal microperforation and a new infiltrative mass at T10-11 with spinal narrowing and vertebral destruction. Vertebral biopsy found non-necrotizing granulomas and numerous acid-fast bacilli (AFB). Targeted DNA sequencing of the colon biopsy confirmed colonic TB. A diagnosis of disseminated TB was made, and the patient was started on targeted antibiotic therapy with good effect.
Discussion: We present a case of disseminated TB, first noted on colonoscopy. While in developed countries, extrapulmonary manifestations can occur in up to a third of TB patients, with the abdomen being the most common site, luminal TB is uncommon. Such instances most often involve the ileocecal region due to the higher concentration of lymphoid tissue and relative luminal stasis. The endoscopic findings of ulcerations and noncontiguous nodular inflammation, with chronic active colitis and granulomas on pathology—as in this patient—can make differentiation from Crohn’s disease difficult. However, a broad differential of infectious mimickers should be considered in atypical cases or in those not responsive to initial therapies. Only a minority of biopsies have AFB on initial pathology, and granulomas are noted in less than half of cases, often delaying diagnosis. Rather, DNA sequencing of tissue has high sensitivity and may be crucial in diagnosing rare causes of colitis. Early TB identification and antibiotic initiation often quickly resolves gastrointestinal symptoms and leads to reduced dissemination and morbidity.
Disclosures:
Max L. Goldman, MD, Brenton G. Davis, MD, Lyle Shlager, MD. P3741 - Hiding in Plain Sight: Colonic Tuberculosis Mimicking Crohn’s Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Kaiser Permanente, San Francisco, CA
Introduction: Colonic tuberculosis (TB) is rare in immunocompetent patients, and diagnosis is often delayed due to its similar appearance on endoscopy and pathology relative to more common diseases. We present a case of colonic TB masquerading as Crohn’s disease.
Case Description/Methods: A healthy 73-year-old man from Southeast Asia presented with a week of abdominal pain, diarrhea, and decreased appetite without fever or leukocytosis. A CT abdomen revealed cecal mural thickening and enhancement. He was discharged on empiric antibiotic treatment for diverticulitis. He represented 2 weeks later with similar symptoms and unchanged CT findings. An expedited colonoscopy was notable for an ulcerated cecal tip and ascending colonic skip lesions and nodularity. Pathology revealed chronic active colitis with ulcers and granulomas. All stains were negative for microorganisms. Ferritin was 500ng/mL, CRP 6.5mg/dL, and QuantiFERON-TB negative. The patient returned to the hospital with signs of peritonism. A repeat CT revealed a cecal microperforation and a new infiltrative mass at T10-11 with spinal narrowing and vertebral destruction. Vertebral biopsy found non-necrotizing granulomas and numerous acid-fast bacilli (AFB). Targeted DNA sequencing of the colon biopsy confirmed colonic TB. A diagnosis of disseminated TB was made, and the patient was started on targeted antibiotic therapy with good effect.
Discussion: We present a case of disseminated TB, first noted on colonoscopy. While in developed countries, extrapulmonary manifestations can occur in up to a third of TB patients, with the abdomen being the most common site, luminal TB is uncommon. Such instances most often involve the ileocecal region due to the higher concentration of lymphoid tissue and relative luminal stasis. The endoscopic findings of ulcerations and noncontiguous nodular inflammation, with chronic active colitis and granulomas on pathology—as in this patient—can make differentiation from Crohn’s disease difficult. However, a broad differential of infectious mimickers should be considered in atypical cases or in those not responsive to initial therapies. Only a minority of biopsies have AFB on initial pathology, and granulomas are noted in less than half of cases, often delaying diagnosis. Rather, DNA sequencing of tissue has high sensitivity and may be crucial in diagnosing rare causes of colitis. Early TB identification and antibiotic initiation often quickly resolves gastrointestinal symptoms and leads to reduced dissemination and morbidity.
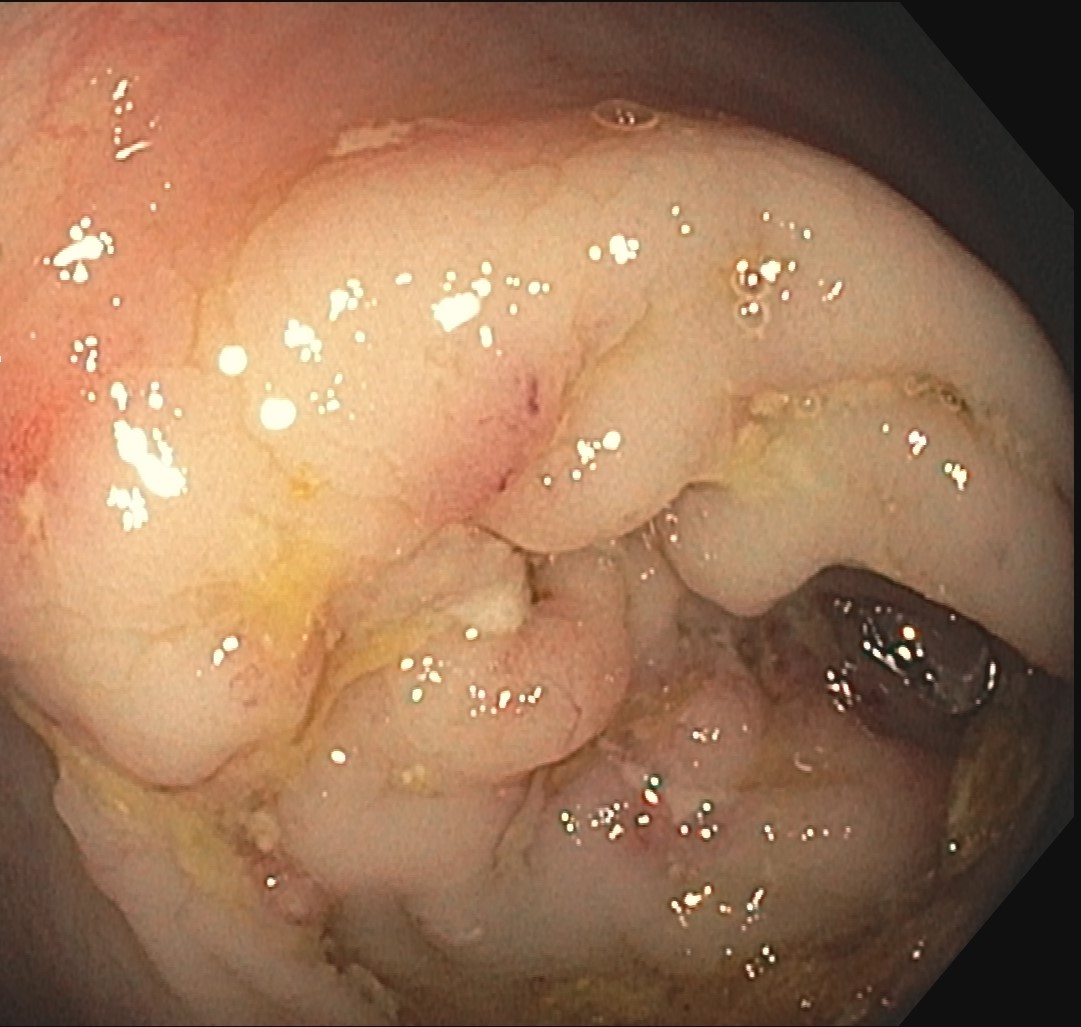
Figure: Figure 1: Unusual inflammation, nodularity, and ulceration in the cecal tip, noted on endoscopy
Disclosures:
Max Goldman: Eli Lilly – Stock-publicly held company(excluding mutual/index funds). Madrigal – Stock-publicly held company(excluding mutual/index funds). Novo Nordisk – Stock-publicly held company(excluding mutual/index funds).
Brenton Davis indicated no relevant financial relationships.
Lyle Shlager indicated no relevant financial relationships.
Max L. Goldman, MD, Brenton G. Davis, MD, Lyle Shlager, MD. P3741 - Hiding in Plain Sight: Colonic Tuberculosis Mimicking Crohn’s Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
