Tuesday Poster Session
Category: Colon
P3764 - Colonic Intussusception Associated With Glucagon-Like Peptide-1 Receptor Agonist Use
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Joseph Gunderson
University of Arizona College of Medicine
Tucson, AZ
Presenting Author(s)
Joseph Gunderson, 1, Elise Le Cam, MD2, Malini Chauhan, MD2, Sara Fallahi, MD1, Sasha Taleban, MD3
1University of Arizona College of Medicine, Tucson, AZ; 2Banner - University of Arizona, Tucson, AZ; 3University of Arizona, Tucson, AZ
Introduction: Glucagon-like peptide-1 receptor agonists (GLP-1RA) have been identified as a risk factor for small and large bowel obstruction (LBO), prompting the Food and Drug Administration to add a warning to GLP-1RA labels in October 2023. Colonic intussusception (CI) is a rare cause of LBO in adults, comprises less than 5% of all intussusception cases, and is typically linked to underlying malignancy. We describe the first reported case of CI leading to LBO in the setting of recent GLP-1RA initiation.
Case Description/Methods: A 39-year-old male with ileocolonic Crohn’s disease in remission, Williams syndrome, congestive heart failure, and type 2 diabetes on semaglutide for 4 months presented with 3 days of worsening loose stools and then 1-2 days of nausea, vomiting, and constipation. His caregiver reported symptoms of diarrhea around the same time that self-resolved. The patient was tachycardic and endorsed severe lower abdominal pain. Abdominal computed tomography (CT) scan showed a 14 cm segment of circumferential bowel wall thickening and mucosal edema along the descending and sigmoid colon with upstream dilation to 5.6 cm. Fluid resuscitation and nasogastric decompression were started, and the patient was admitted for concern of partial, mechanical LBO.
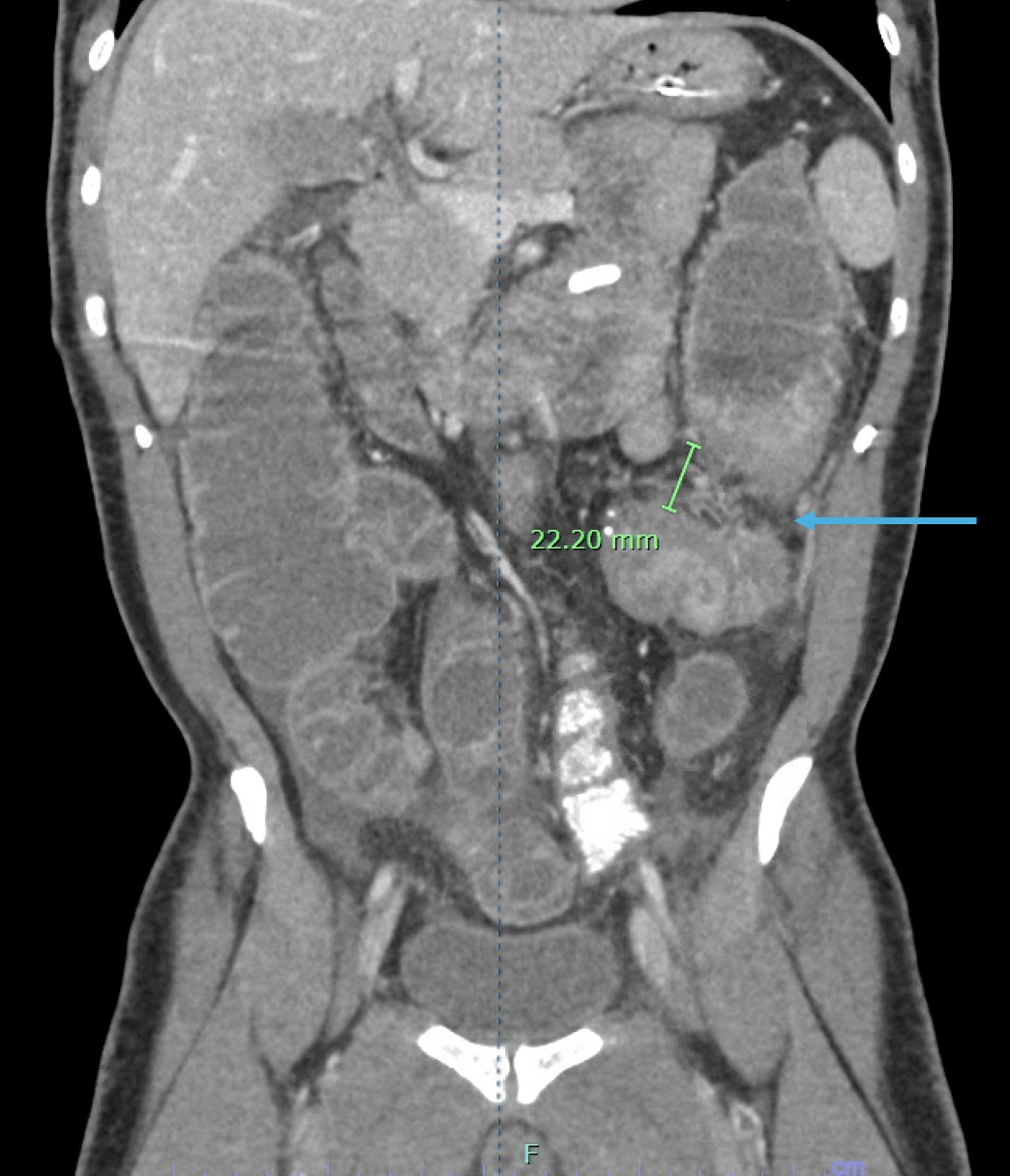
The following day, the patient developed progression of abdominal distention, vomiting, and obstipation. A gastrografin enema indicated a LBO at the sigmoid-descending colon. Repeat contrast abdominal CT suggested a possible 2.2 cm CI in the descending colon. Emergent laparotomy revealed a phlegmonous mass of descending colon telescoping into the sigmoid colon. The 16-cm segment of the involved bowel was resected, and end-to-end anastomosis was performed. Surgical pathology showed three 0.5 cm and one 1.8 cm inflammatory polyps without malignancy or active Crohn’s disease.
The patient regained bowel function on postoperative day 3 and required total parenteral nutrition for 14 days. He was discharged home on postoperative day 16.
Discussion: This case illustrates LBO due to CI in the setting of a GLP-1RA, viral gastroenteritis, and inflammatory polyps. GLP-1RAs have been linked to small bowel intussusception, but this is the first reported case implicating GLP-1RA involvement in CI. While a possible role of the patient’s inflammatory polyps or viral gastroenteritis cannot be excluded, reported cases of adult CI due to polyps involve larger, adenomatous lesions, and intussusception due to viral gastroenteritis has not been reported in adults.
Disclosures:
Joseph Gunderson, 1, Elise Le Cam, MD2, Malini Chauhan, MD2, Sara Fallahi, MD1, Sasha Taleban, MD3. P3764 - Colonic Intussusception Associated With Glucagon-Like Peptide-1 Receptor Agonist Use, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Arizona College of Medicine, Tucson, AZ; 2Banner - University of Arizona, Tucson, AZ; 3University of Arizona, Tucson, AZ
Introduction: Glucagon-like peptide-1 receptor agonists (GLP-1RA) have been identified as a risk factor for small and large bowel obstruction (LBO), prompting the Food and Drug Administration to add a warning to GLP-1RA labels in October 2023. Colonic intussusception (CI) is a rare cause of LBO in adults, comprises less than 5% of all intussusception cases, and is typically linked to underlying malignancy. We describe the first reported case of CI leading to LBO in the setting of recent GLP-1RA initiation.
Case Description/Methods: A 39-year-old male with ileocolonic Crohn’s disease in remission, Williams syndrome, congestive heart failure, and type 2 diabetes on semaglutide for 4 months presented with 3 days of worsening loose stools and then 1-2 days of nausea, vomiting, and constipation. His caregiver reported symptoms of diarrhea around the same time that self-resolved. The patient was tachycardic and endorsed severe lower abdominal pain. Abdominal computed tomography (CT) scan showed a 14 cm segment of circumferential bowel wall thickening and mucosal edema along the descending and sigmoid colon with upstream dilation to 5.6 cm. Fluid resuscitation and nasogastric decompression were started, and the patient was admitted for concern of partial, mechanical LBO.
The following day, the patient developed progression of abdominal distention, vomiting, and obstipation. A gastrografin enema indicated a LBO at the sigmoid-descending colon. Repeat contrast abdominal CT suggested a possible 2.2 cm CI in the descending colon. Emergent laparotomy revealed a phlegmonous mass of descending colon telescoping into the sigmoid colon. The 16-cm segment of the involved bowel was resected, and end-to-end anastomosis was performed. Surgical pathology showed three 0.5 cm and one 1.8 cm inflammatory polyps without malignancy or active Crohn’s disease.
The patient regained bowel function on postoperative day 3 and required total parenteral nutrition for 14 days. He was discharged home on postoperative day 16.
Discussion: This case illustrates LBO due to CI in the setting of a GLP-1RA, viral gastroenteritis, and inflammatory polyps. GLP-1RAs have been linked to small bowel intussusception, but this is the first reported case implicating GLP-1RA involvement in CI. While a possible role of the patient’s inflammatory polyps or viral gastroenteritis cannot be excluded, reported cases of adult CI due to polyps involve larger, adenomatous lesions, and intussusception due to viral gastroenteritis has not been reported in adults.
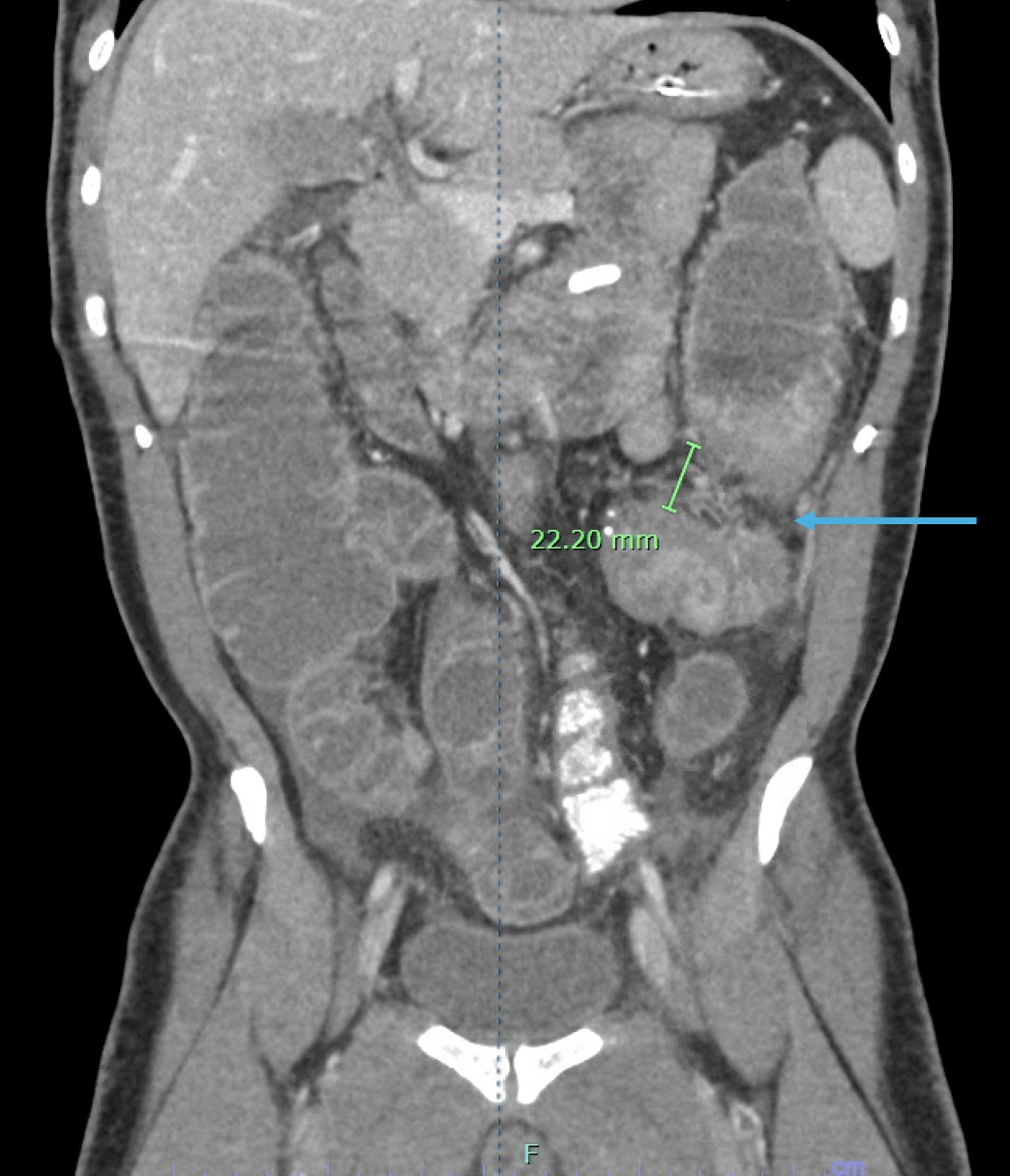
Figure: Figure 1. Abdominal CT scan showing colonic intussusception at the descending colon with surrounding bowel wall edema.
Disclosures:
Joseph Gunderson indicated no relevant financial relationships.
Elise Le Cam indicated no relevant financial relationships.
Malini Chauhan indicated no relevant financial relationships.
Sara Fallahi indicated no relevant financial relationships.
Sasha Taleban: AbbVie – Advisory Committee/Board Member. Bristol Myers Squibb – Grant/Research Support. Eli Lilly – Grant/Research Support. Janssen – Grant/Research Support. Pfizer – Grant/Research Support. Takeda – Grant/Research Support.
Joseph Gunderson, 1, Elise Le Cam, MD2, Malini Chauhan, MD2, Sara Fallahi, MD1, Sasha Taleban, MD3. P3764 - Colonic Intussusception Associated With Glucagon-Like Peptide-1 Receptor Agonist Use, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

