Tuesday Poster Session
Category: Colon
P3796 - When a Routine Polypectomy Reveals an Unexpected Finding
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Carla M. Cepero-Jimenez, MD
VA Caribbean Healthcare System
San Juan, PR
Presenting Author(s)
Carla M. Cepero-Jimenez, MD, Juan G. Feliciano Figueroa, MD, Kathia Rosado-Orozco, MD, Andres Rabell-Bernal, MD
VA Caribbean Healthcare System, San Juan, Puerto Rico
Introduction: Marginal zone lymphoma is a non-Hodgkin lymphoma (NHL) subtype that appears to emerge from post-germinal center marginal zone B-cells. One of its subtypes is extranodal marginal zone lymphoma of mucosal associated lymphoid tissue (MALT lymphoma) which is uncommon and accounts for approximately 5 to 10% of NHL in the United States. Extranodal MALT lymphoma predominantly involves the gastrointestinal (GI) tract, and the stomach is the most common site of involvement followed by the small bowel and colon. Colonic MALT lymphoma involvement is rare and accounts for less than 0.5% of all colon cancers. In this case, we present a case of MALT lymphoma found in multiple colon polyps in an elderly male patient.
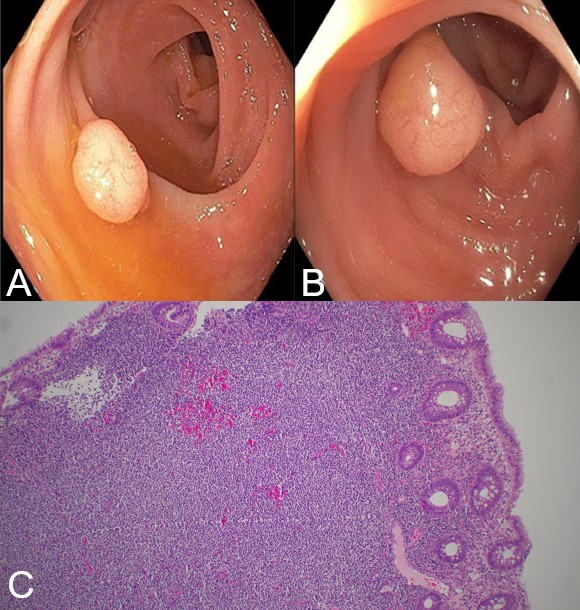
Case Description/Methods: 82-year-old male with a history of atrial fibrillation on apixaban, hypertension, hypothyroidism, among other comorbidities who underwent a surveillance colonoscopy that was remarkable for large external hemorrhoids, pandiverticulosis, and 6 colon polyps that were removed. Pathology initially revealed 1 tubular adenoma, 1 tubular adenoma with one focus of dense lymphoid infiltrate, and 4 polyps with colonic mucosa with a dense lymphoid infiltrate. Given these findings, pathology was further analyzed and showed extranodal MALT lymphoma. PET/CT showed mildly hypermetabolic subcentimeter lymph nodes at bilateral inguinal and external iliac compartments.
Discussion: Extranodal MALT lymphoma most commonly involves the stomach but can be seen in other parts of the gut, lungs, salivary glands, thyroid, ocular adnexa, breast, soft tissues, among others. The median age of diagnosis is 60 years and some studies have shown twice the incidence in females than in males. Several predisposing conditions associated with GI lymphoma include: H. pylori infection, autoimmune diseases, inflammatory bowel disease, celiac disease, immunosuppression, among others. Although gastric MALT lymphoma has a strong association with H. pylori, no association has been seen with colonic MALT. Most cases of colonic MALT lymphoma present with GI bleeding and can rarely cause intestinal obstruction, abdominal pain, perforation, or intussusception. Other patients, like in this case, can be asymptomatic and diagnosis can be made from polyp resection. Endoscopic findings can range from normal appearing mucosa to an ulcer or polypoid lesion. Awareness of this entity is important as it can present in different ways and given the rarity, there are no standard guidelines for treatment.
Disclosures:
Carla M. Cepero-Jimenez, MD, Juan G. Feliciano Figueroa, MD, Kathia Rosado-Orozco, MD, Andres Rabell-Bernal, MD. P3796 - When a Routine Polypectomy Reveals an Unexpected Finding, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
VA Caribbean Healthcare System, San Juan, Puerto Rico
Introduction: Marginal zone lymphoma is a non-Hodgkin lymphoma (NHL) subtype that appears to emerge from post-germinal center marginal zone B-cells. One of its subtypes is extranodal marginal zone lymphoma of mucosal associated lymphoid tissue (MALT lymphoma) which is uncommon and accounts for approximately 5 to 10% of NHL in the United States. Extranodal MALT lymphoma predominantly involves the gastrointestinal (GI) tract, and the stomach is the most common site of involvement followed by the small bowel and colon. Colonic MALT lymphoma involvement is rare and accounts for less than 0.5% of all colon cancers. In this case, we present a case of MALT lymphoma found in multiple colon polyps in an elderly male patient.
Case Description/Methods: 82-year-old male with a history of atrial fibrillation on apixaban, hypertension, hypothyroidism, among other comorbidities who underwent a surveillance colonoscopy that was remarkable for large external hemorrhoids, pandiverticulosis, and 6 colon polyps that were removed. Pathology initially revealed 1 tubular adenoma, 1 tubular adenoma with one focus of dense lymphoid infiltrate, and 4 polyps with colonic mucosa with a dense lymphoid infiltrate. Given these findings, pathology was further analyzed and showed extranodal MALT lymphoma. PET/CT showed mildly hypermetabolic subcentimeter lymph nodes at bilateral inguinal and external iliac compartments.
Discussion: Extranodal MALT lymphoma most commonly involves the stomach but can be seen in other parts of the gut, lungs, salivary glands, thyroid, ocular adnexa, breast, soft tissues, among others. The median age of diagnosis is 60 years and some studies have shown twice the incidence in females than in males. Several predisposing conditions associated with GI lymphoma include: H. pylori infection, autoimmune diseases, inflammatory bowel disease, celiac disease, immunosuppression, among others. Although gastric MALT lymphoma has a strong association with H. pylori, no association has been seen with colonic MALT. Most cases of colonic MALT lymphoma present with GI bleeding and can rarely cause intestinal obstruction, abdominal pain, perforation, or intussusception. Other patients, like in this case, can be asymptomatic and diagnosis can be made from polyp resection. Endoscopic findings can range from normal appearing mucosa to an ulcer or polypoid lesion. Awareness of this entity is important as it can present in different ways and given the rarity, there are no standard guidelines for treatment.
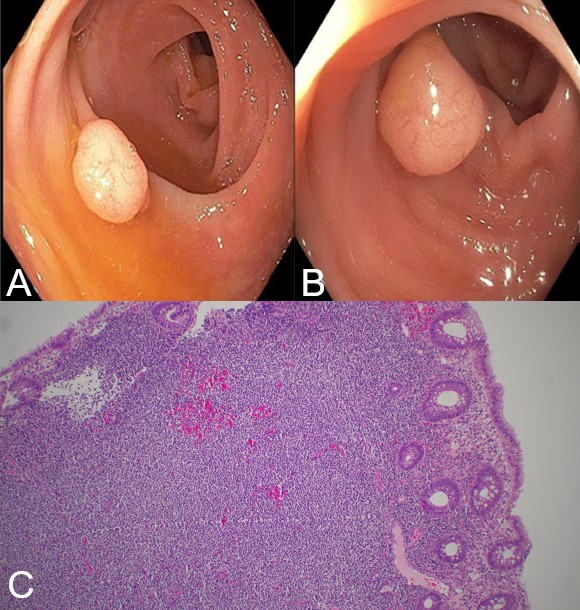
Figure: Extranodal MALT lymphoma seen as polyps in colonoscopy (A&B). Colonic mucosa with foci of a dense monotonous lymphoid infiltrate composed of monocytoid cells (C). Immunostains showed most of the lymphocytes are CD 20 positive B cells which co-expressed CD23 and bcl-2 with a low Ki-67 proliferation index. Germinal center cells were positive for CD10 and bcl-6, CD3, CD5 and CD43.
Disclosures:
Carla Cepero-Jimenez indicated no relevant financial relationships.
Juan Feliciano Figueroa indicated no relevant financial relationships.
Kathia Rosado-Orozco indicated no relevant financial relationships.
Andres Rabell-Bernal indicated no relevant financial relationships.
Carla M. Cepero-Jimenez, MD, Juan G. Feliciano Figueroa, MD, Kathia Rosado-Orozco, MD, Andres Rabell-Bernal, MD. P3796 - When a Routine Polypectomy Reveals an Unexpected Finding, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
