Tuesday Poster Session
Category: Colon
P3798 - Progression of Eosinophilic Esophagitis to Eosinophilic Gastroenteritis
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- SK
Shaheera Kamal, MD
University of Texas Health Science Center
Tyler, TX
Presenting Author(s)
Shaheera Kamal, MD1, Ian Naron, MD1, Muhammad Majeed, MD2
1University of Texas Health Science Center, Tyler, TX; 2UT Health East Texas Digestive Disease Center, Tyler, TX
Introduction: Eosinophilic gastroenteritis (EGE) is a rare disease that current studies estimate has a prevalence ranging from 8.4 to 28 patients per 100,000. EGE has a bimodal age distribution typically affecting the pediatric population and adults between their third and fifth decade of life. EGE occurs due to dysfunction of the immune system leading to cytokine and interleukin release that leads to an inflammatory response by eosinophils within the gastrointestinal tract.
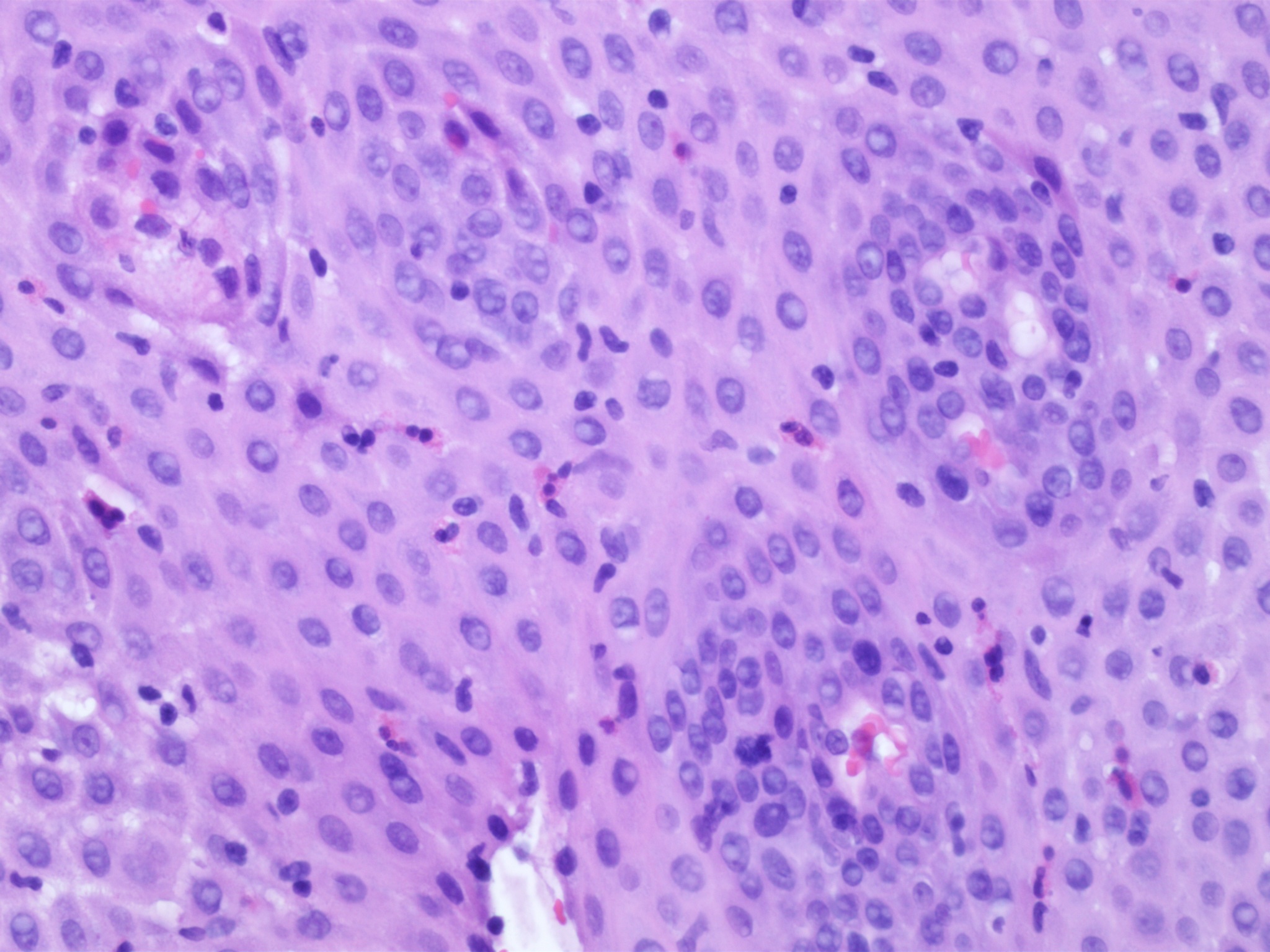
Case Description/Methods: We present the case of a 67-year-old female with a past medical history of eosinophilic esophagitis (EOE) who presented with non-bloody vomiting, abdominal pain, and non-bloody diarrhea for 2 months. Patient was compliant with oral pantoprazole for management of EOE and her disease was thought to be in remission. Her physical examination revealed tachycardia, normal blood pressure, and generalized abdominal tenderness without rebound. The initial workup showed peripheral eosinophilia, normal lactate, and colon wall thickening in the splenic flexure. Clostridium difficile and stool ova/parasite examinations were negative. Due to the location of colon wall thickening in the watershed area, there was concern for ischemic colitis, but peripheral eosinophilia, past medical history and upper GI symptoms pointed to an eosinophilic disorder. Due to high suspicion for eosinophilic disorder, inpatient EGD and colonoscopy was performed. Endoscopic workup showed mucosal edema in the distal gastric body, the second portion of the duodenum, and the left colon. Biopsies from the esophagus, stomach, duodenum, and colon showed eosinophilic infiltration throughout the gastrointestinal tract, concerning for EGE (Figure 1.). The patient was started on Prednisone 40mg daily, leading to a dramatic improvement in symptoms within 48 hours. She was discharged home with follow-up in 2 weeks. The patient was scheduled for a repeat endoscopy in 4 weeks to assess the improvement in eosinophilic infiltration.
Discussion: This case underscores the significance of a keeping a high suspicion of index for eosinophilic disorders in high risk patients. Inpatient diagnostic endoscopy with biopsy of abnormal appearing mucosa play a vital role in early diagnosis and reduce hospital stay. Inflammatory bowel disease, parasitic infection, systemic vasculitis, and systemic mastocytosis should be ruled out. Steroids (budesonide, prednisone) are the mainstay of therapy during acute exacerbations. The disease can present with a relapsing-remitting pattern.
Disclosures:
Shaheera Kamal, MD1, Ian Naron, MD1, Muhammad Majeed, MD2. P3798 - Progression of Eosinophilic Esophagitis to Eosinophilic Gastroenteritis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Texas Health Science Center, Tyler, TX; 2UT Health East Texas Digestive Disease Center, Tyler, TX
Introduction: Eosinophilic gastroenteritis (EGE) is a rare disease that current studies estimate has a prevalence ranging from 8.4 to 28 patients per 100,000. EGE has a bimodal age distribution typically affecting the pediatric population and adults between their third and fifth decade of life. EGE occurs due to dysfunction of the immune system leading to cytokine and interleukin release that leads to an inflammatory response by eosinophils within the gastrointestinal tract.
Case Description/Methods: We present the case of a 67-year-old female with a past medical history of eosinophilic esophagitis (EOE) who presented with non-bloody vomiting, abdominal pain, and non-bloody diarrhea for 2 months. Patient was compliant with oral pantoprazole for management of EOE and her disease was thought to be in remission. Her physical examination revealed tachycardia, normal blood pressure, and generalized abdominal tenderness without rebound. The initial workup showed peripheral eosinophilia, normal lactate, and colon wall thickening in the splenic flexure. Clostridium difficile and stool ova/parasite examinations were negative. Due to the location of colon wall thickening in the watershed area, there was concern for ischemic colitis, but peripheral eosinophilia, past medical history and upper GI symptoms pointed to an eosinophilic disorder. Due to high suspicion for eosinophilic disorder, inpatient EGD and colonoscopy was performed. Endoscopic workup showed mucosal edema in the distal gastric body, the second portion of the duodenum, and the left colon. Biopsies from the esophagus, stomach, duodenum, and colon showed eosinophilic infiltration throughout the gastrointestinal tract, concerning for EGE (Figure 1.). The patient was started on Prednisone 40mg daily, leading to a dramatic improvement in symptoms within 48 hours. She was discharged home with follow-up in 2 weeks. The patient was scheduled for a repeat endoscopy in 4 weeks to assess the improvement in eosinophilic infiltration.
Discussion: This case underscores the significance of a keeping a high suspicion of index for eosinophilic disorders in high risk patients. Inpatient diagnostic endoscopy with biopsy of abnormal appearing mucosa play a vital role in early diagnosis and reduce hospital stay. Inflammatory bowel disease, parasitic infection, systemic vasculitis, and systemic mastocytosis should be ruled out. Steroids (budesonide, prednisone) are the mainstay of therapy during acute exacerbations. The disease can present with a relapsing-remitting pattern.
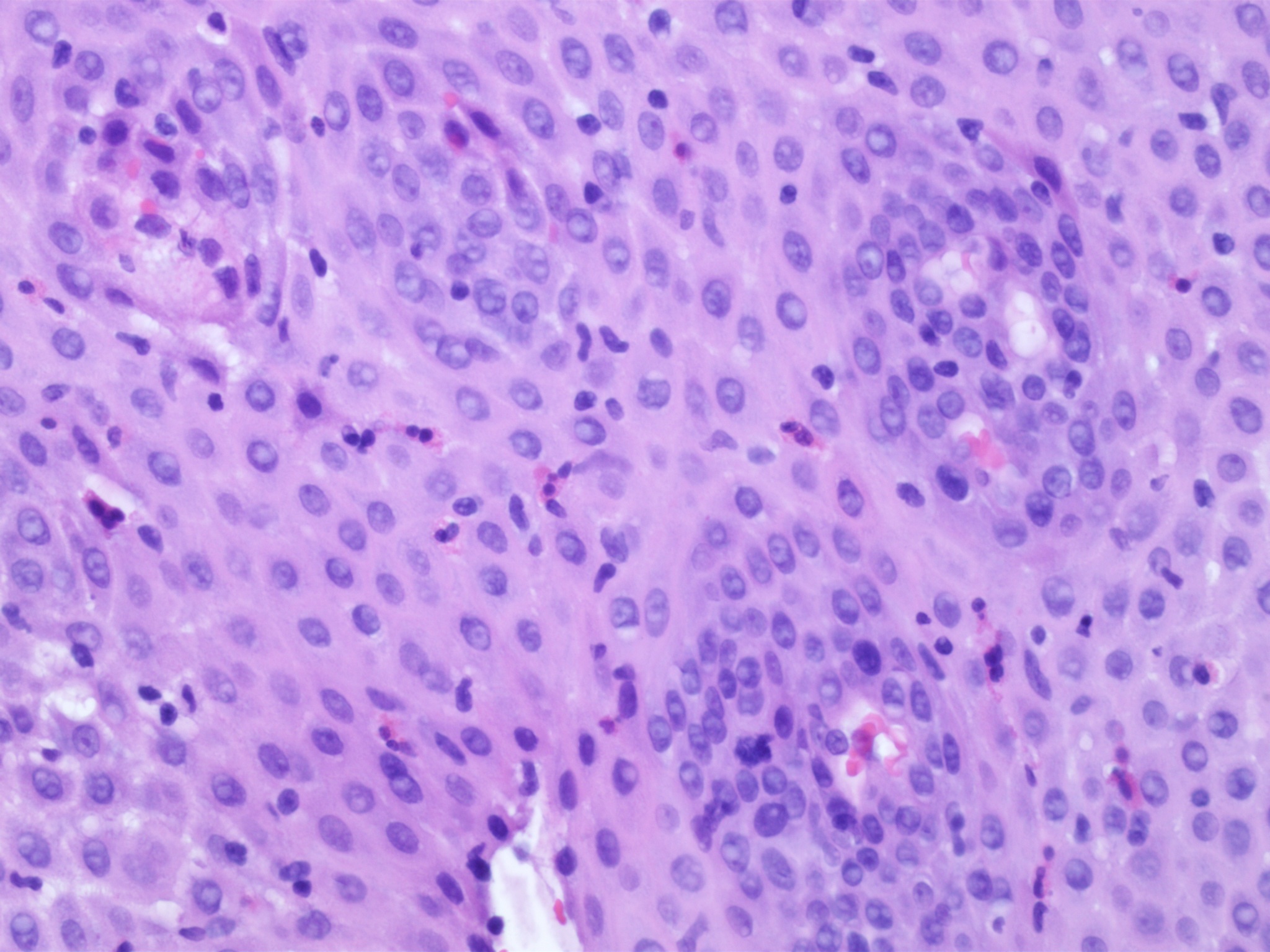
Figure: Figure 1. Left colon histopathology revealing increased eosinophils
Disclosures:
Shaheera Kamal indicated no relevant financial relationships.
Ian Naron indicated no relevant financial relationships.
Muhammad Majeed indicated no relevant financial relationships.
Shaheera Kamal, MD1, Ian Naron, MD1, Muhammad Majeed, MD2. P3798 - Progression of Eosinophilic Esophagitis to Eosinophilic Gastroenteritis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
