Tuesday Poster Session
Category: Colon
P3800 - Gastrointestinal Manifestations of Plasmablastic Lymphoma: A Case Series from a Tertiary Cancer Center
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Michael Gianarakis, MD
University of Illinois at Chicago
Chicago, IL
Presenting Author(s)
Michael Gianarakis, MD1, Syed Shahrukh Rizvi, DO2, Hasan S. Raza, MD3, Elie Ghoulam, MD4, Robert E.. Carroll, MD1
1University of Illinois at Chicago, Chicago, IL; 2University of Illinois College of Medicine, Chicago, IL; 3University of Illinois, Chicago, IL; 4Quincy Medical Group, Quincy, IL
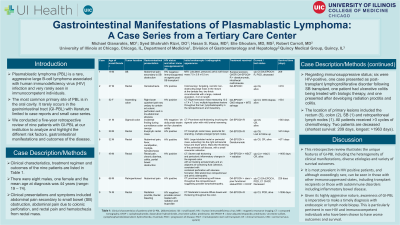
Introduction: Plasmablastic lymphoma (PBL) is a rare, aggressive large B-cell lymphoma associated with human immunodeficiency virus (HIV) infection and very rarely seen in immunocompetent individuals. The most common primary site of PBL is in the oral cavity. It rarely occurs in the gastrointestinal tract (GI-PBL) with literature limited to case reports and small case series. We conducted a five-year retrospective review of nine patients with GI-PBL at our institution to analyze and highlight the different risk factors, gastrointestinal manifestations and outcomes of the disease.
Case Description/Methods: Clinical characteristics, treatment regimen and outcomes of the nine patients are listed in Table 1. There were eight males, one female and the mean age at diagnosis was 44 years (range: 19 – 74). Clinical presentations and symptoms included abdominal pain secondary to small bowel (SB) obstruction, abdominal pain due to colonic perforation, and rectal pain and hematochezia from rectal mass. Regarding immunosuppressive status; six were HIV-positive, one case presented as post-transplant lymphoproliferative disorder following SB transplant, one patient had ulcerative colitis being treated with biologic therapy, and one presented after developing radiation proctitis and colitis. The location of primary lesions included the rectum (5), colon (2), SB (1) and retroperitoneal lymph nodes (1). All patients received >3 cycles of chemotherapy. Two patients are deceased (shortest survival: 209 days, longest: >1963 days).
Discussion: This retrospective review illustrates the unique features of GI-PBL including the heterogeneity of clinical manifestations, diverse etiologies and variety of survival outcomes. It is most prevalent in HIV positive patients, and although exceedingly rare, can be seen in those with other immunosuppressed states, including transplant recipients or those with autoimmune disorders including inflammatory bowel disease. Given its highly aggressive nature, awareness of GI-PBL is imperative in order to make a timely diagnosis with endoscopic or lymph node biopsy. This is particularly pertinent in non-HIV and immunocompetent individuals who have been shown to have worse outcomes and survival.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Michael Gianarakis, MD1, Syed Shahrukh Rizvi, DO2, Hasan S. Raza, MD3, Elie Ghoulam, MD4, Robert E.. Carroll, MD1. P3800 - Gastrointestinal Manifestations of Plasmablastic Lymphoma: A Case Series from a Tertiary Cancer Center, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Illinois at Chicago, Chicago, IL; 2University of Illinois College of Medicine, Chicago, IL; 3University of Illinois, Chicago, IL; 4Quincy Medical Group, Quincy, IL
Introduction: Plasmablastic lymphoma (PBL) is a rare, aggressive large B-cell lymphoma associated with human immunodeficiency virus (HIV) infection and very rarely seen in immunocompetent individuals. The most common primary site of PBL is in the oral cavity. It rarely occurs in the gastrointestinal tract (GI-PBL) with literature limited to case reports and small case series. We conducted a five-year retrospective review of nine patients with GI-PBL at our institution to analyze and highlight the different risk factors, gastrointestinal manifestations and outcomes of the disease.
Case Description/Methods: Clinical characteristics, treatment regimen and outcomes of the nine patients are listed in Table 1. There were eight males, one female and the mean age at diagnosis was 44 years (range: 19 – 74). Clinical presentations and symptoms included abdominal pain secondary to small bowel (SB) obstruction, abdominal pain due to colonic perforation, and rectal pain and hematochezia from rectal mass. Regarding immunosuppressive status; six were HIV-positive, one case presented as post-transplant lymphoproliferative disorder following SB transplant, one patient had ulcerative colitis being treated with biologic therapy, and one presented after developing radiation proctitis and colitis. The location of primary lesions included the rectum (5), colon (2), SB (1) and retroperitoneal lymph nodes (1). All patients received >3 cycles of chemotherapy. Two patients are deceased (shortest survival: 209 days, longest: >1963 days).
Discussion: This retrospective review illustrates the unique features of GI-PBL including the heterogeneity of clinical manifestations, diverse etiologies and variety of survival outcomes. It is most prevalent in HIV positive patients, and although exceedingly rare, can be seen in those with other immunosuppressed states, including transplant recipients or those with autoimmune disorders including inflammatory bowel disease. Given its highly aggressive nature, awareness of GI-PBL is imperative in order to make a timely diagnosis with endoscopic or lymph node biopsy. This is particularly pertinent in non-HIV and immunocompetent individuals who have been shown to have worse outcomes and survival.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Michael Gianarakis indicated no relevant financial relationships.
Syed Shahrukh Rizvi indicated no relevant financial relationships.
Hasan Raza indicated no relevant financial relationships.
Elie Ghoulam indicated no relevant financial relationships.
Robert Carroll indicated no relevant financial relationships.
Michael Gianarakis, MD1, Syed Shahrukh Rizvi, DO2, Hasan S. Raza, MD3, Elie Ghoulam, MD4, Robert E.. Carroll, MD1. P3800 - Gastrointestinal Manifestations of Plasmablastic Lymphoma: A Case Series from a Tertiary Cancer Center, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

