Tuesday Poster Session
Category: Colon
P3802 - A Hidden Danger: GI Perforation Presenting as Pneumomediastinum in Chronic Corticosteroid User
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Nancy Mayer, DO
Riverside Medical Center
Bourbonnais, IL
Presenting Author(s)
Nancy Mayer, DO, Trisha Andrews, MD
Riverside Medical Center, Bourbonnais, IL
Introduction: Pneumomediastinum and subcutaneous emphysema are typically seen in alveolar rupture. Gastrointestinal origin is extremely rare and carries a high mortality rate. Unfortunately, patients on chronic corticosteroids may not exhibit symptoms that are promptly recognized as a bowel perforation. We present a case of a perforated bowel presenting with pneumomediastinum and subcutaneous emphysema in a patient on chronic corticosteroids.
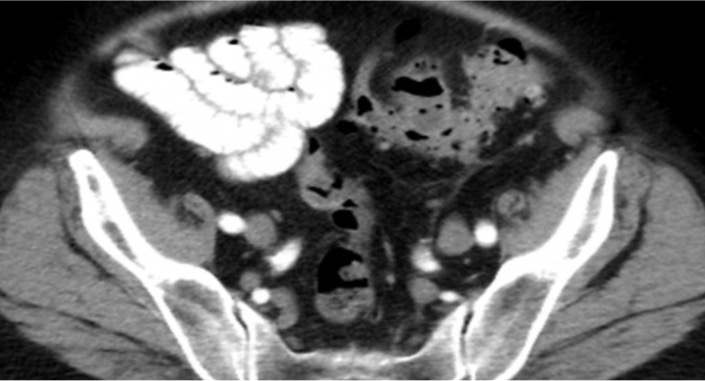
Case Description/Methods: A 63-year-old male with rheumatoid arthritis on chronic prednisone presented with a complaint of shortness of breath and neck swelling. Physical examination revealed crepitus and bloating of the neck. Urgent imaging showed extensive pneumomediastinum extending inferiorly with subcutaneous emphysema in the abdominal wall. Work up with CT esophagram was unrevealing. His respiratory status remained stable, and he was discharged the following day. However, he returned to the hospital one week later with hemodynamic instability and new infectious symptoms. He was empirically treated for mediastinitis with broad-spectrum antibiotics. Further imaging revealed a 3.1cm loculated fluid collection adjacent to the sigmoid colon with extravasation of gas into the adjacent subcutaneous space. A diagnosis of perforated diverticulitis with abscess and subcutaneous fistula was made. The patient underwent a sigmoid colectomy and was discharged three days postoperatively.
Discussion: Fewer than 20 cases of pneumomediastinum due to colonic perforation, excluding iatrogenic and traumatic injury, exist in the literature. Of these cases, only four patients presented without abdominal pain. Notably, all were on chronic corticosteroids or immunosuppressants. In patients on 20mg/day or more of steroid therapy, symptoms of peritonitis due to perforation may be subtle or absent. Mortality rates of gastrointestinal perforation are 13.3% for those on 20mg/day or less of steroids but rise to 85.1% for those on higher doses, partly due to delayed intervention. This patient, on 25mg of prednisone daily, showed no signs of abdominal pain or peritonitis. This masking effect is due to the anti-inflammatory and immunosuppressive properties of corticosteroids which reduce signs of inflammation, such as pain and fever, making perforation difficult to detect. Chronic corticosteroid use can mask the abdominal symptoms of bowel perforation, necessitating a high index of suspicion in patients with subcutaneous emphysema or pneumomediastinum who are on long-term corticosteroid therapy.
Disclosures:
Nancy Mayer, DO, Trisha Andrews, MD. P3802 - A Hidden Danger: GI Perforation Presenting as Pneumomediastinum in Chronic Corticosteroid User, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Riverside Medical Center, Bourbonnais, IL
Introduction: Pneumomediastinum and subcutaneous emphysema are typically seen in alveolar rupture. Gastrointestinal origin is extremely rare and carries a high mortality rate. Unfortunately, patients on chronic corticosteroids may not exhibit symptoms that are promptly recognized as a bowel perforation. We present a case of a perforated bowel presenting with pneumomediastinum and subcutaneous emphysema in a patient on chronic corticosteroids.
Case Description/Methods: A 63-year-old male with rheumatoid arthritis on chronic prednisone presented with a complaint of shortness of breath and neck swelling. Physical examination revealed crepitus and bloating of the neck. Urgent imaging showed extensive pneumomediastinum extending inferiorly with subcutaneous emphysema in the abdominal wall. Work up with CT esophagram was unrevealing. His respiratory status remained stable, and he was discharged the following day. However, he returned to the hospital one week later with hemodynamic instability and new infectious symptoms. He was empirically treated for mediastinitis with broad-spectrum antibiotics. Further imaging revealed a 3.1cm loculated fluid collection adjacent to the sigmoid colon with extravasation of gas into the adjacent subcutaneous space. A diagnosis of perforated diverticulitis with abscess and subcutaneous fistula was made. The patient underwent a sigmoid colectomy and was discharged three days postoperatively.
Discussion: Fewer than 20 cases of pneumomediastinum due to colonic perforation, excluding iatrogenic and traumatic injury, exist in the literature. Of these cases, only four patients presented without abdominal pain. Notably, all were on chronic corticosteroids or immunosuppressants. In patients on 20mg/day or more of steroid therapy, symptoms of peritonitis due to perforation may be subtle or absent. Mortality rates of gastrointestinal perforation are 13.3% for those on 20mg/day or less of steroids but rise to 85.1% for those on higher doses, partly due to delayed intervention. This patient, on 25mg of prednisone daily, showed no signs of abdominal pain or peritonitis. This masking effect is due to the anti-inflammatory and immunosuppressive properties of corticosteroids which reduce signs of inflammation, such as pain and fever, making perforation difficult to detect. Chronic corticosteroid use can mask the abdominal symptoms of bowel perforation, necessitating a high index of suspicion in patients with subcutaneous emphysema or pneumomediastinum who are on long-term corticosteroid therapy.
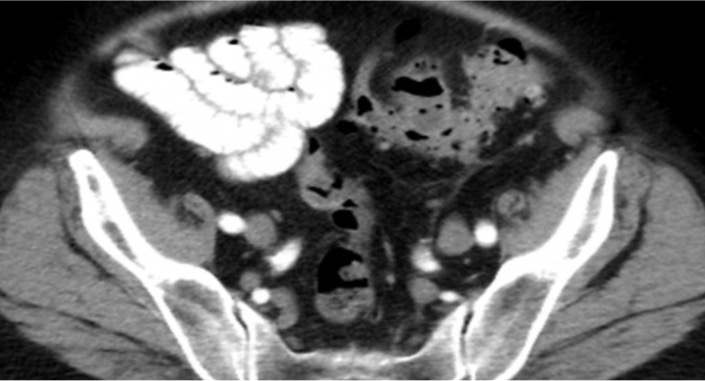
Figure: Extraluminal gas and fluid collection compatible with sigmoid perforation and abscess
Disclosures:
Nancy Mayer indicated no relevant financial relationships.
Trisha Andrews indicated no relevant financial relationships.
Nancy Mayer, DO, Trisha Andrews, MD. P3802 - A Hidden Danger: GI Perforation Presenting as Pneumomediastinum in Chronic Corticosteroid User, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
