Tuesday Poster Session
Category: Colon
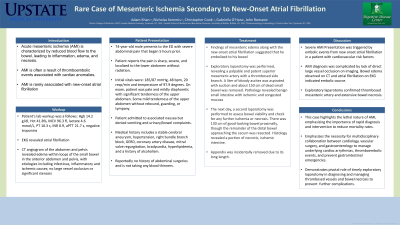
P3805 - Rare Case of Mesenteric Ischemia Secondary to New-Onset Atrial Fibrillation
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- AK
Adam M. Khan
SUNY Upstate Medical University
syracue, NY
Presenting Author(s)
Adam Khan, 1, Christopher Cook, 2, Nicholas Kemmis, 3, John Romano, MD4, Gabriella O'Hara, 4
1SUNY Upstate Medical University, Manlius, NY; 2SUNY Upstate Medical University, North Syracuse, NY; 3University of Buffalo Jacobs School of Medicine, Jamesville, NY; 4Gastroenterology and Hepatology of CNY, Jamesville, NY
Introduction: Acute mesenteric ischemia (AMI) represents a medical emergency characterized by compromised blood flow to the bowel, resulting in inflammation, edema, and eventual tissue necrosis. With mortality rates ranging from 60% to 80%, its prompt diagnosis and management are imperative. AMI frequently stems from thromboembolic events associated with cardiac abnormalities. Here, we present a case wherein AMI developed in a patient with new-onset atrial fibrillation (AF) and resulting thromboembolic event, underscoring the necessity for vigilance in patients presenting with cardiac symptoms and abdominal pain to improve outcomes through timely intervention.
Case Description/Methods: A 74-year-old male presented with severe, localized abdominal pain and a history significant for cerebral artery aneurysm, hypertension, coronary artery disease, bradycardia, mitral valve regurgitation, and right bundle branch block, but no anticoagulation therapy. On exam, the patient was pale and mildly diaphoretic with significant tenderness of the lower abdomen, in particular, some mild tenderness of the upper abdomen without rebound, guarding or tympany. Diagnostic workup revealed signs of AMI, including elevated lactate levels and an EKG indicative of AF. CT imaging demonstrated bowel edema, suggesting embolic etiology. He was then prepared for an emergency exploratory laparotomy. Anticoagulation with heparin was considered but ultimately postponed until after the operation. Surgical exploration confirmed thrombosed mesenteric artery branches and extensive bowel necrosis, necessitating resection of about 150 cm of dead small bowel. Subsequent management involved anticoagulation therapy with coumadin and outpatient follow-up.
Discussion: This case highlights a severe presentation of AMI secondary to thromboembolic events, likely triggered by new-onset AF. Diagnostic challenges included the absence of direct vessel occlusion on imaging, emphasizing the importance of clinical suspicion guided by imaging and EKG findings. Prompt surgical intervention was pivotal in confirming the diagnosis and preventing further ischemic damage. Overall, this case underscores the critical need for a multidisciplinary approach, timely intervention, and stringent anticoagulation management in patients with AF to mitigate the risk of AMI and its associated morbidity and mortality.
Disclosures:
Adam Khan, 1, Christopher Cook, 2, Nicholas Kemmis, 3, John Romano, MD4, Gabriella O'Hara, 4. P3805 - Rare Case of Mesenteric Ischemia Secondary to New-Onset Atrial Fibrillation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1SUNY Upstate Medical University, Manlius, NY; 2SUNY Upstate Medical University, North Syracuse, NY; 3University of Buffalo Jacobs School of Medicine, Jamesville, NY; 4Gastroenterology and Hepatology of CNY, Jamesville, NY
Introduction: Acute mesenteric ischemia (AMI) represents a medical emergency characterized by compromised blood flow to the bowel, resulting in inflammation, edema, and eventual tissue necrosis. With mortality rates ranging from 60% to 80%, its prompt diagnosis and management are imperative. AMI frequently stems from thromboembolic events associated with cardiac abnormalities. Here, we present a case wherein AMI developed in a patient with new-onset atrial fibrillation (AF) and resulting thromboembolic event, underscoring the necessity for vigilance in patients presenting with cardiac symptoms and abdominal pain to improve outcomes through timely intervention.
Case Description/Methods: A 74-year-old male presented with severe, localized abdominal pain and a history significant for cerebral artery aneurysm, hypertension, coronary artery disease, bradycardia, mitral valve regurgitation, and right bundle branch block, but no anticoagulation therapy. On exam, the patient was pale and mildly diaphoretic with significant tenderness of the lower abdomen, in particular, some mild tenderness of the upper abdomen without rebound, guarding or tympany. Diagnostic workup revealed signs of AMI, including elevated lactate levels and an EKG indicative of AF. CT imaging demonstrated bowel edema, suggesting embolic etiology. He was then prepared for an emergency exploratory laparotomy. Anticoagulation with heparin was considered but ultimately postponed until after the operation. Surgical exploration confirmed thrombosed mesenteric artery branches and extensive bowel necrosis, necessitating resection of about 150 cm of dead small bowel. Subsequent management involved anticoagulation therapy with coumadin and outpatient follow-up.
Discussion: This case highlights a severe presentation of AMI secondary to thromboembolic events, likely triggered by new-onset AF. Diagnostic challenges included the absence of direct vessel occlusion on imaging, emphasizing the importance of clinical suspicion guided by imaging and EKG findings. Prompt surgical intervention was pivotal in confirming the diagnosis and preventing further ischemic damage. Overall, this case underscores the critical need for a multidisciplinary approach, timely intervention, and stringent anticoagulation management in patients with AF to mitigate the risk of AMI and its associated morbidity and mortality.
Disclosures:
Adam Khan indicated no relevant financial relationships.
Christopher Cook indicated no relevant financial relationships.
Nicholas Kemmis indicated no relevant financial relationships.
John Romano indicated no relevant financial relationships.
Gabriella O'Hara indicated no relevant financial relationships.
Adam Khan, 1, Christopher Cook, 2, Nicholas Kemmis, 3, John Romano, MD4, Gabriella O'Hara, 4. P3805 - Rare Case of Mesenteric Ischemia Secondary to New-Onset Atrial Fibrillation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
