Tuesday Poster Session
Category: Colorectal Cancer Prevention
P3869 - Quality Indicators of Endoscopists for Baseline and Surveillance Colonoscopy are Associated With Risk of Metachronous Colorectal Neoplasia
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Aasma Shaukat, MD, MPH, FACG
Robert M. and Mary H. Glickman Professor of Medicine; Professor of Population Health; Director, GI Outcomes Research
NYU Langone Health
New York, NY
Presenting Author(s)
Aasma Shaukat, MD, MPH1, Peter Liang, MD, MPH2, Mohammad Bilal, MD3, Seth Gross, MD2, Jennifer Holub, MA, MPH4, Mark Pochapin, MD, MPH1
1NYU, New York, NY; 2NYU Langone Health, New York, NY; 3University of Minnesota and Minneapolis VA Health Care System, Minneapolis, MN; 4GI Quality Improvement Consortium, Ltd., Bethesda, MD
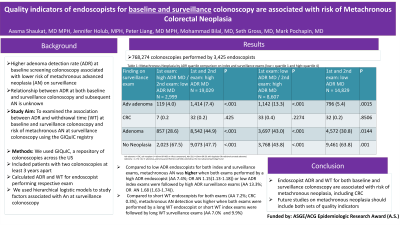
Introduction: An association between higher adenoma detection rate (ADR) at baseline screening colonoscopy and lower risk of metachronous advanced neoplasia (AN, defined as CRC or advanced adenoma (AA)) has been reported. However, the relationship between ADR at both baseline and surveillance colonoscopy and subsequent AN is unknown. We examined the association between ADR and withdrawal time (WT) at baseline and surveillance colonoscopy and risk of metachronous AN at surveillance colonoscopy.
Methods: We used GIQuIC, a repository of colonoscopies across the US. Each patient has a unique ID at a participating site. Endoscopist NPI are associated with each exam. We included patients with two colonoscopies at least 3 years apart (index and surveillance) between 2011 and 2022 and calculated the ADR and WT for the endoscopist performing the respective exams. We built a multivariable logistic regression model with metachronous AN as the outcome and ADR and WT as independent variables, controlling for patient age, sex and race.
Results: We included 768,274 patients and 3,425 endoscopists. Mean patient age was 61 years and 48% were male; 66% were White and 3% were Hispanic. Indication for index colonoscopy were screening (43.4%), surveillance (39.0%) and diagnostic (17.6%). ADR quartiles were ≤29.7%, >29.7%-37.2%, >37.2%-45.0% and >45%. WT quartiles were ≤7.06 min, >7.06-8.16 min, >8.16-9.7min, >9.7min. AA detection was lowest when low ADR endoscopists performed both index and surveillance exams (5.4%, Table 1) and high ADR index exams were followed by low ADR surveillance exams (4.0%). Compared to low ADR endoscopists for both index and surveillance exams, metachronous AN was significantly higher when both exams performed by a high ADR endoscopist (AA 7.4%; OR for AN 1.15(1.13-1.18)) or low ADR index exams were followed by high ADR surveillance exams (AA 13.3%; OR for AN 1.68 (1.63-1.74)). Compared to short WT endoscopists for both exams (AA 7.0%; CRC 0.3%), metachronous AA detection was higher when both exams were performed by a long WT endoscopist or short WT index exams were followed by long WT surveillance exams (AA 7.7% and 9.9%, P< 0.001) but similar CRC detection of 0.2% and 0.2% (p 0.14).
Discussion: Our findings show endoscopist ADR and WT for both baseline and surveillance colonoscopy are associated with risk of metachronous neoplasia, including CRC. Future studies on metachronous neoplasia should include both sets of quality indicators.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Aasma Shaukat, MD, MPH1, Peter Liang, MD, MPH2, Mohammad Bilal, MD3, Seth Gross, MD2, Jennifer Holub, MA, MPH4, Mark Pochapin, MD, MPH1. P3869 - Quality Indicators of Endoscopists for Baseline and Surveillance Colonoscopy are Associated With Risk of Metachronous Colorectal Neoplasia, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1NYU, New York, NY; 2NYU Langone Health, New York, NY; 3University of Minnesota and Minneapolis VA Health Care System, Minneapolis, MN; 4GI Quality Improvement Consortium, Ltd., Bethesda, MD
Introduction: An association between higher adenoma detection rate (ADR) at baseline screening colonoscopy and lower risk of metachronous advanced neoplasia (AN, defined as CRC or advanced adenoma (AA)) has been reported. However, the relationship between ADR at both baseline and surveillance colonoscopy and subsequent AN is unknown. We examined the association between ADR and withdrawal time (WT) at baseline and surveillance colonoscopy and risk of metachronous AN at surveillance colonoscopy.
Methods: We used GIQuIC, a repository of colonoscopies across the US. Each patient has a unique ID at a participating site. Endoscopist NPI are associated with each exam. We included patients with two colonoscopies at least 3 years apart (index and surveillance) between 2011 and 2022 and calculated the ADR and WT for the endoscopist performing the respective exams. We built a multivariable logistic regression model with metachronous AN as the outcome and ADR and WT as independent variables, controlling for patient age, sex and race.
Results: We included 768,274 patients and 3,425 endoscopists. Mean patient age was 61 years and 48% were male; 66% were White and 3% were Hispanic. Indication for index colonoscopy were screening (43.4%), surveillance (39.0%) and diagnostic (17.6%). ADR quartiles were ≤29.7%, >29.7%-37.2%, >37.2%-45.0% and >45%. WT quartiles were ≤7.06 min, >7.06-8.16 min, >8.16-9.7min, >9.7min. AA detection was lowest when low ADR endoscopists performed both index and surveillance exams (5.4%, Table 1) and high ADR index exams were followed by low ADR surveillance exams (4.0%). Compared to low ADR endoscopists for both index and surveillance exams, metachronous AN was significantly higher when both exams performed by a high ADR endoscopist (AA 7.4%; OR for AN 1.15(1.13-1.18)) or low ADR index exams were followed by high ADR surveillance exams (AA 13.3%; OR for AN 1.68 (1.63-1.74)). Compared to short WT endoscopists for both exams (AA 7.0%; CRC 0.3%), metachronous AA detection was higher when both exams were performed by a long WT endoscopist or short WT index exams were followed by long WT surveillance exams (AA 7.7% and 9.9%, P< 0.001) but similar CRC detection of 0.2% and 0.2% (p 0.14).
Discussion: Our findings show endoscopist ADR and WT for both baseline and surveillance colonoscopy are associated with risk of metachronous neoplasia, including CRC. Future studies on metachronous neoplasia should include both sets of quality indicators.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Aasma Shaukat indicated no relevant financial relationships.
Peter Liang: Freenome – Grant/Research Support. Guardant Health – Advisory Committee/Board Member. Natera – Advisory Committee/Board Member.
Mohammad Bilal: Boston Scientific – Consultant. Cook endoscopy – Speakers Bureau.
Seth Gross: Cook – Consultant. Medtronic – Consultant. Microtech – Consultant. Olympis – Consultant. Provation – Consultant.
Jennifer Holub indicated no relevant financial relationships.
Mark Pochapin indicated no relevant financial relationships.
Aasma Shaukat, MD, MPH1, Peter Liang, MD, MPH2, Mohammad Bilal, MD3, Seth Gross, MD2, Jennifer Holub, MA, MPH4, Mark Pochapin, MD, MPH1. P3869 - Quality Indicators of Endoscopists for Baseline and Surveillance Colonoscopy are Associated With Risk of Metachronous Colorectal Neoplasia, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
