Tuesday Poster Session
Category: Colorectal Cancer Prevention
P3870 - Enhancing Diversity and Inclusion in the PREEMPT CRC Study Through Strategic Site Selection and Innovative Recruitment Tools
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Aasma Shaukat, MD, MPH, FACG
Robert M. and Mary H. Glickman Professor of Medicine; Professor of Population Health; Director, GI Outcomes Research
NYU Langone Health
New York, NY
Presenting Author(s)
Aasma Shaukat, MD, MPH1, Karolina Kutnik, MS2, Kristen Petersen, 3, Chuanbo Xu, PhD4, Lilian C. Lee, PhD5, Lance Baldo, MD5, Theodore R. Levin, MD, MS, FACG6
1NYU Langone Health, New York, NY; 2Freenome, Los Angeles, CA; 3Freenome, Brisbane, CA; 4Freenome, Inc., South San Francisco, CA; 5Freenome, South San Francisco, CA; 6Kaiser Permanente, Pleasanton, CA
Introduction: Diversity in clinical studies is crucial for ensuring the study population reflects the intended patient demographic. The PREEMPT CRC study, a prospective, double-blinded, multi-center observational study, supported the clinical validation of an investigational blood-based test to provide a convenient option for colorectal cancer (CRC) screening. Freenome’s blood test met all co-primary endpoints, demonstrating 79.2% sensitivity for CRC and 91.5% specificity for non-advanced colorectal neoplasia. The study enrolled a diverse population that reflected various ethnic, racial, and geographical backgrounds in the U.S. This analysis provides additional perspective on the study population and explores the methodology used to contribute to a diverse study population.
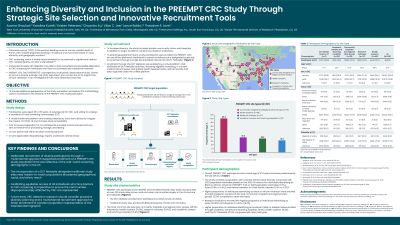
Methods: The study enrolled participants aged 45-85 at average CRC risk. Eligible and consenting participants underwent a blood draw followed by standard of care screening colonoscopy. The blood sample was assessed with an investigational blood-based CRC screening test. To ensure diversity, the study included smaller sites and community hospitals beyond large academic institutions. The study also used a decentralized clinical trial (DCT) model to expand geographical reach, implemented electronic consenting and mobile phlebotomy services.
Results: The study enrolled 48,995 participants, achieving ethnic/racial diversity similar to the 2020 U.S. Census for Blacks (11.2% vs. 13.6%), Asians (6.8% vs. 6.3%) and Native Hawaiian or Other Pacific Islander (0.3% vs. 0.4%). Types of sites that contributed to the study were community hospitals and regional clinics (n=91), health systems (n=40), research institutes (n=37), academic centers/teaching hospitals (n=32) and a DCT metasite. Community clinics and academic centers enrolled the highest proportion of Black participants (12.1% and 21.4%, respectively), while research institutions had the highest proportion of Asian (24.8%) and Hispanic/Latinx (18.3%) populations. The DCT metasite enrolled 12,137 participants (24.7% of total) from 49 U.S. states.
Discussion: PREEMPT CRC integrated multiple recruitment methods to enhance inclusivity. This multimodal approach ensured diversified representation through inclusion of sites with harder-to-reach populations, which was reflected in ethnic, racial and geographical data. The study underscores the importance of early diversity planning and using multiple methods to broaden the representation of the patient population.
Disclosures:
Aasma Shaukat, MD, MPH1, Karolina Kutnik, MS2, Kristen Petersen, 3, Chuanbo Xu, PhD4, Lilian C. Lee, PhD5, Lance Baldo, MD5, Theodore R. Levin, MD, MS, FACG6. P3870 - Enhancing Diversity and Inclusion in the PREEMPT CRC Study Through Strategic Site Selection and Innovative Recruitment Tools, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1NYU Langone Health, New York, NY; 2Freenome, Los Angeles, CA; 3Freenome, Brisbane, CA; 4Freenome, Inc., South San Francisco, CA; 5Freenome, South San Francisco, CA; 6Kaiser Permanente, Pleasanton, CA
Introduction: Diversity in clinical studies is crucial for ensuring the study population reflects the intended patient demographic. The PREEMPT CRC study, a prospective, double-blinded, multi-center observational study, supported the clinical validation of an investigational blood-based test to provide a convenient option for colorectal cancer (CRC) screening. Freenome’s blood test met all co-primary endpoints, demonstrating 79.2% sensitivity for CRC and 91.5% specificity for non-advanced colorectal neoplasia. The study enrolled a diverse population that reflected various ethnic, racial, and geographical backgrounds in the U.S. This analysis provides additional perspective on the study population and explores the methodology used to contribute to a diverse study population.
Methods: The study enrolled participants aged 45-85 at average CRC risk. Eligible and consenting participants underwent a blood draw followed by standard of care screening colonoscopy. The blood sample was assessed with an investigational blood-based CRC screening test. To ensure diversity, the study included smaller sites and community hospitals beyond large academic institutions. The study also used a decentralized clinical trial (DCT) model to expand geographical reach, implemented electronic consenting and mobile phlebotomy services.
Results: The study enrolled 48,995 participants, achieving ethnic/racial diversity similar to the 2020 U.S. Census for Blacks (11.2% vs. 13.6%), Asians (6.8% vs. 6.3%) and Native Hawaiian or Other Pacific Islander (0.3% vs. 0.4%). Types of sites that contributed to the study were community hospitals and regional clinics (n=91), health systems (n=40), research institutes (n=37), academic centers/teaching hospitals (n=32) and a DCT metasite. Community clinics and academic centers enrolled the highest proportion of Black participants (12.1% and 21.4%, respectively), while research institutions had the highest proportion of Asian (24.8%) and Hispanic/Latinx (18.3%) populations. The DCT metasite enrolled 12,137 participants (24.7% of total) from 49 U.S. states.
Discussion: PREEMPT CRC integrated multiple recruitment methods to enhance inclusivity. This multimodal approach ensured diversified representation through inclusion of sites with harder-to-reach populations, which was reflected in ethnic, racial and geographical data. The study underscores the importance of early diversity planning and using multiple methods to broaden the representation of the patient population.
Disclosures:
Aasma Shaukat: iterative health; Freenome – Consultant.
Karolina Kutnik: Freenome – Employee.
Kristen Petersen: Invitae Corporation – Employee.
Chuanbo Xu indicated no relevant financial relationships.
Lilian C. Lee: Freenome – Employee.
Lance Baldo: Freenome – Employee, Stock Options.
Theodore Levin: Freenome, Inc – Grant/Research Support.
Aasma Shaukat, MD, MPH1, Karolina Kutnik, MS2, Kristen Petersen, 3, Chuanbo Xu, PhD4, Lilian C. Lee, PhD5, Lance Baldo, MD5, Theodore R. Levin, MD, MS, FACG6. P3870 - Enhancing Diversity and Inclusion in the PREEMPT CRC Study Through Strategic Site Selection and Innovative Recruitment Tools, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
