Tuesday Poster Session
Category: Esophagus
P3905 - Racial Differences in Incidence and Prevalence of Barrett’s Esophagus
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- MJ
Mikaela Nikkola Jara-Tantoco, MD, MS
Einstein Healthcare Network
Philadelphia, PA
Presenting Author(s)
Mikaela Nikkola Jara-Tantoco, MD, MS1, Abiodun Idowu, MD2, Carlo Gabriel C. Casipit, MD3, Karecia Byfield, MBBS3, Blanche Echikunwoke, MD3, Kevin Bryan Lo, MD4, Michael L. Davis, DO3
1Einstein Healthcare Network, Philadelphia, PA; 2Jefferson Einstein Hospital, Philadelphia, PA; 3Albert Einstein Medical Center, Philadelphia, PA; 4Brigham and Women's Hospital, Harvard Medical School, Boston, MA
Introduction: One of the risk factors considered in screening for Barrett’s esophagus (BE) is race. This study aims to look at real-world data in determining the incidence and prevalence of BE in different racial groups.
Methods: TriNetX, a large global research network of deidentified electronic health records, was queried on June 12, 2024. A cohort of adults (at least 50 years old and above) with a diagnosis of gastroesophageal reflux disease (GERD) preceding esophagogastroduodenoscopy (EGD) by at least five years from January 1, 2020 to December 31, 2023 was used for this study. Chi-square test was done for evaluating racial differences of incidence and prevalence, with the white race as reference.
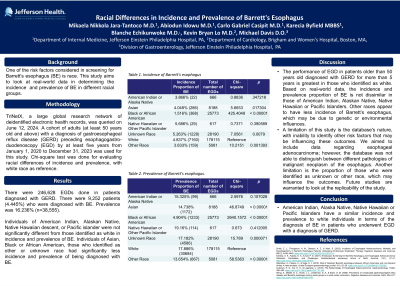
Results: There were 246,628 EGDs done in patients diagnosed with GERD. There were 9,252 patients (4.445%) who were diagnosed with BE. Prevalence was 16.236% (n=38,555).
Individuals of American Indian, Alaskan Native, Native Hawaiian, or Pacific islander descent were not significantly different from those identified as white in incidence and prevalence of BE. Individuals of Asian, Black or African American descent, and those who identified as other or unknown race had significantly less incidence and prevalence of being diagnosed with BE.
Discussion: The performance of EGD in patients older than 50 years old diagnosed with GERD for more than 5 years is greatest in those who identified as white. Based on real-world data, the incidence and prevalence proportion of BE is not dissimilar in those of American Indian, Alaskan Native, Native Hawaiian or Pacific Islanders. Other races appear to have less incidence of Barrett’s esophagus, which may be due to genetic or environmental influences.
A limitation of this study is the database's nature, with inability to identify other risk factors that may be influencing these outcomes, such as socioeconomic issues. We aimed to include data regarding esophageal adenocarcinoma; however, the database was not able to distinguish between different pathologies of malignant neoplasm of the esophagus. Another limitation is the proportion of those who were identified as unknown or other race, which may influence the outcomes. Future studies are warranted to look at the replicability of the study.
In conclusion, American Indian, Alaska Native, Native Hawaiian or Pacific Islanders have a similar incidence and prevalence to white individuals in terms of the diagnosis of BE in patients who underwent EGD with a diagnosis of GERD.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Mikaela Nikkola Jara-Tantoco, MD, MS1, Abiodun Idowu, MD2, Carlo Gabriel C. Casipit, MD3, Karecia Byfield, MBBS3, Blanche Echikunwoke, MD3, Kevin Bryan Lo, MD4, Michael L. Davis, DO3. P3905 - Racial Differences in Incidence and Prevalence of Barrett’s Esophagus, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Einstein Healthcare Network, Philadelphia, PA; 2Jefferson Einstein Hospital, Philadelphia, PA; 3Albert Einstein Medical Center, Philadelphia, PA; 4Brigham and Women's Hospital, Harvard Medical School, Boston, MA
Introduction: One of the risk factors considered in screening for Barrett’s esophagus (BE) is race. This study aims to look at real-world data in determining the incidence and prevalence of BE in different racial groups.
Methods: TriNetX, a large global research network of deidentified electronic health records, was queried on June 12, 2024. A cohort of adults (at least 50 years old and above) with a diagnosis of gastroesophageal reflux disease (GERD) preceding esophagogastroduodenoscopy (EGD) by at least five years from January 1, 2020 to December 31, 2023 was used for this study. Chi-square test was done for evaluating racial differences of incidence and prevalence, with the white race as reference.
Results: There were 246,628 EGDs done in patients diagnosed with GERD. There were 9,252 patients (4.445%) who were diagnosed with BE. Prevalence was 16.236% (n=38,555).
Individuals of American Indian, Alaskan Native, Native Hawaiian, or Pacific islander descent were not significantly different from those identified as white in incidence and prevalence of BE. Individuals of Asian, Black or African American descent, and those who identified as other or unknown race had significantly less incidence and prevalence of being diagnosed with BE.
Discussion: The performance of EGD in patients older than 50 years old diagnosed with GERD for more than 5 years is greatest in those who identified as white. Based on real-world data, the incidence and prevalence proportion of BE is not dissimilar in those of American Indian, Alaskan Native, Native Hawaiian or Pacific Islanders. Other races appear to have less incidence of Barrett’s esophagus, which may be due to genetic or environmental influences.
A limitation of this study is the database's nature, with inability to identify other risk factors that may be influencing these outcomes, such as socioeconomic issues. We aimed to include data regarding esophageal adenocarcinoma; however, the database was not able to distinguish between different pathologies of malignant neoplasm of the esophagus. Another limitation is the proportion of those who were identified as unknown or other race, which may influence the outcomes. Future studies are warranted to look at the replicability of the study.
In conclusion, American Indian, Alaska Native, Native Hawaiian or Pacific Islanders have a similar incidence and prevalence to white individuals in terms of the diagnosis of BE in patients who underwent EGD with a diagnosis of GERD.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Mikaela Nikkola Jara-Tantoco indicated no relevant financial relationships.
Abiodun Idowu indicated no relevant financial relationships.
Carlo Gabriel Casipit indicated no relevant financial relationships.
Karecia Byfield indicated no relevant financial relationships.
Blanche Echikunwoke indicated no relevant financial relationships.
Kevin Bryan Lo indicated no relevant financial relationships.
Michael Davis indicated no relevant financial relationships.
Mikaela Nikkola Jara-Tantoco, MD, MS1, Abiodun Idowu, MD2, Carlo Gabriel C. Casipit, MD3, Karecia Byfield, MBBS3, Blanche Echikunwoke, MD3, Kevin Bryan Lo, MD4, Michael L. Davis, DO3. P3905 - Racial Differences in Incidence and Prevalence of Barrett’s Esophagus, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
