Tuesday Poster Session
Category: Esophagus
P3916 - An Association Between Lymphocytic Esophagitis and Inflammatory Bowel Disease: Fact or Fiction?
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- LL
Laura E. Lavette, MD
University of Virginia Medical Center
Charlottesville, VA
Presenting Author(s)
Laura E. Lavette, MD, Sahil Khanna, MD, Chris Young, MD, Calvin Geng, MD, Amanda Gibbs, MD, Anne Mills, MD, Edward Stelow, MD, Andrew Copland, MD
University of Virginia Medical Center, Charlottesville, VA
Introduction: There are conflicting reports surrounding the association between Lymphocytic Esophagitis (LE) and other gastrointestinal diseases. Rubio et al was the first to suggest a relationship between LE and Crohn’s.1 Two years later, the University of Michigan published a review of 42 cases and found no association between LE and Inflammatory Bowel Disease (IBD).2 There is more robust literature supporting a link between LE and IBD in the pediatric population.3 Given these disparities, we aimed to further characterize the relationship between LE and IBD at a single tertiary academic center.
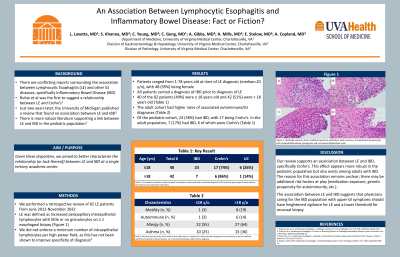
Methods: We performed a retrospective review of 82 LE patients from June 2012-Nov 2022. LE was defined as increased peripapillary intraepithelial lymphocytes with little or no granulocytes on ≥1 esophageal biopsy; we did not enforce a minimum number of intraepithelial lymphocytes per high power field, as this has not been shown to improve specificity of diagnosis.4
Results: Patients ranged from ages 1-78 at time of LE diagnosis, with the majority (59%) being female. 40 of the 82 patients (49%) were ≤18 years old and 42 (51%) were >18. Of the pediatric cohort, 23 (57.5%) had IBD, with 17 (74%) being Crohn’s. In the adult population, 7 (17%) had IBD, 6 (86%) of which were Crohn’s. All patients carried a diagnosis of IBD prior to diagnosis of LE.
Discussion: Our review supports an association between LE and IBD, specifically Crohn’s. This effect appears more robust in the pediatric population but also exists amongst adults with IBD. The reason for this association remains unclear; there may be additional risk factors (genetic propensity for autoimmunity, medication exposure, etc.) at play. The association between LE and IBD suggests that physicians caring for the IBD population with upper GI symptoms should have heightened vigilance for LE and a lower threshold for mucosal biopsy.
1. Rubio, Carlos, et al. Lymphocytic esophagitis: a histologic subset of chronic esophagitis. Am J Clin Pathol. 2006 Mar;125(3):432–7.
2. Purdy JK, et al. Lymphocytic Esophagitis: A Chronic or Recurring Pattern of Esophagitis Resembling Allergic Contact Dermatitis. Am J Clin Pathol. 2008 Oct;130(4):508–13.
3. Ebach DR, et al. Lymphocytic esophagitis: a possible manifestation of pediatric upper gastrointestinal Crohn’s disease. Inflamm Bowel Dis. 2011 Jan;17(1):45–9.
4. Haque S, Genta RM. Lymphocytic oesophagitis: clinicopathological aspects of an emerging condition. Gut. 2012 Aug;61(8):1108–14.
Disclosures:
Laura E. Lavette, MD, Sahil Khanna, MD, Chris Young, MD, Calvin Geng, MD, Amanda Gibbs, MD, Anne Mills, MD, Edward Stelow, MD, Andrew Copland, MD. P3916 - An Association Between Lymphocytic Esophagitis and Inflammatory Bowel Disease: Fact or Fiction?, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
University of Virginia Medical Center, Charlottesville, VA
Introduction: There are conflicting reports surrounding the association between Lymphocytic Esophagitis (LE) and other gastrointestinal diseases. Rubio et al was the first to suggest a relationship between LE and Crohn’s.1 Two years later, the University of Michigan published a review of 42 cases and found no association between LE and Inflammatory Bowel Disease (IBD).2 There is more robust literature supporting a link between LE and IBD in the pediatric population.3 Given these disparities, we aimed to further characterize the relationship between LE and IBD at a single tertiary academic center.
Methods: We performed a retrospective review of 82 LE patients from June 2012-Nov 2022. LE was defined as increased peripapillary intraepithelial lymphocytes with little or no granulocytes on ≥1 esophageal biopsy; we did not enforce a minimum number of intraepithelial lymphocytes per high power field, as this has not been shown to improve specificity of diagnosis.4
Results: Patients ranged from ages 1-78 at time of LE diagnosis, with the majority (59%) being female. 40 of the 82 patients (49%) were ≤18 years old and 42 (51%) were >18. Of the pediatric cohort, 23 (57.5%) had IBD, with 17 (74%) being Crohn’s. In the adult population, 7 (17%) had IBD, 6 (86%) of which were Crohn’s. All patients carried a diagnosis of IBD prior to diagnosis of LE.
Discussion: Our review supports an association between LE and IBD, specifically Crohn’s. This effect appears more robust in the pediatric population but also exists amongst adults with IBD. The reason for this association remains unclear; there may be additional risk factors (genetic propensity for autoimmunity, medication exposure, etc.) at play. The association between LE and IBD suggests that physicians caring for the IBD population with upper GI symptoms should have heightened vigilance for LE and a lower threshold for mucosal biopsy.
1. Rubio, Carlos, et al. Lymphocytic esophagitis: a histologic subset of chronic esophagitis. Am J Clin Pathol. 2006 Mar;125(3):432–7.
2. Purdy JK, et al. Lymphocytic Esophagitis: A Chronic or Recurring Pattern of Esophagitis Resembling Allergic Contact Dermatitis. Am J Clin Pathol. 2008 Oct;130(4):508–13.
3. Ebach DR, et al. Lymphocytic esophagitis: a possible manifestation of pediatric upper gastrointestinal Crohn’s disease. Inflamm Bowel Dis. 2011 Jan;17(1):45–9.
4. Haque S, Genta RM. Lymphocytic oesophagitis: clinicopathological aspects of an emerging condition. Gut. 2012 Aug;61(8):1108–14.
Disclosures:
Laura Lavette indicated no relevant financial relationships.
Sahil Khanna indicated no relevant financial relationships.
Chris Young indicated no relevant financial relationships.
Calvin Geng indicated no relevant financial relationships.
Amanda Gibbs indicated no relevant financial relationships.
Anne Mills indicated no relevant financial relationships.
Edward Stelow indicated no relevant financial relationships.
Andrew Copland indicated no relevant financial relationships.
Laura E. Lavette, MD, Sahil Khanna, MD, Chris Young, MD, Calvin Geng, MD, Amanda Gibbs, MD, Anne Mills, MD, Edward Stelow, MD, Andrew Copland, MD. P3916 - An Association Between Lymphocytic Esophagitis and Inflammatory Bowel Disease: Fact or Fiction?, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
