Tuesday Poster Session
Category: Esophagus
P3928 - Marked Improvement in Esophageal Food Impaction Biopsy Rate (FIBR) After Implementation of a Multicenter Behavioral Intervention
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Walker D. Redd, MD
University of North Carolina at Chapel Hill School of Medicine
Chapel Hill, NC
Presenting Author(s)
Walker D. Redd, MD1, Courtney Richman, MD2, Trevor Barlowe, MD1, Sabrina Layne, MD2, Angel Miro-Gonzalez, MD1, Nirmala Gonsalves, MD3, Evan S.. Dellon, MD, MPH, FACG1, David A. Leiman, MD, MSHP4
1University of North Carolina at Chapel Hill School of Medicine, Chapel Hill, NC; 2Duke University School of Medicine, Durham, NC; 3Feinberg School of Medicine, Northwestern University, Chicago, IL; 4Duke University School of Medicine, Chapel Hill, NC
Introduction: Performing esophageal biopsies at the time of esophageal food impaction (EFI) is a quality indicator in eosinophilic esophagitis (EoE) but is infrequently performed leading to diagnostic delay. We aimed to determine whether a behavioral intervention could improve the food impaction biopsy rate (FIBR) and quality of EFI follow-up care.
Methods: We created a standardized electronic health record (EHR) protocol that could be embedded within the EFI treatment pathway. This algorithm was shared among clinicians and posted in the endoscopy units at four locations across two health systems. We obtained baseline FIBR performance rates among adults undergoing upper endoscopy from 7/1/2021-6/30/2023 and assessed post-intervention outcomes from 10/2/2023-4/2/2024. Patient demographics, clinical, procedural, and management details were extracted from the EHR. The primary outcome was the FIBR, defined as the proportion of patients with esophageal biopsies performed at time of endoscopy for EFI. Patients with impacted nonfood foreign bodies were excluded. Pre- and post-intervention data were compared using bivariate statistics. Data from each center were analyzed separately to assess for replicability of results.
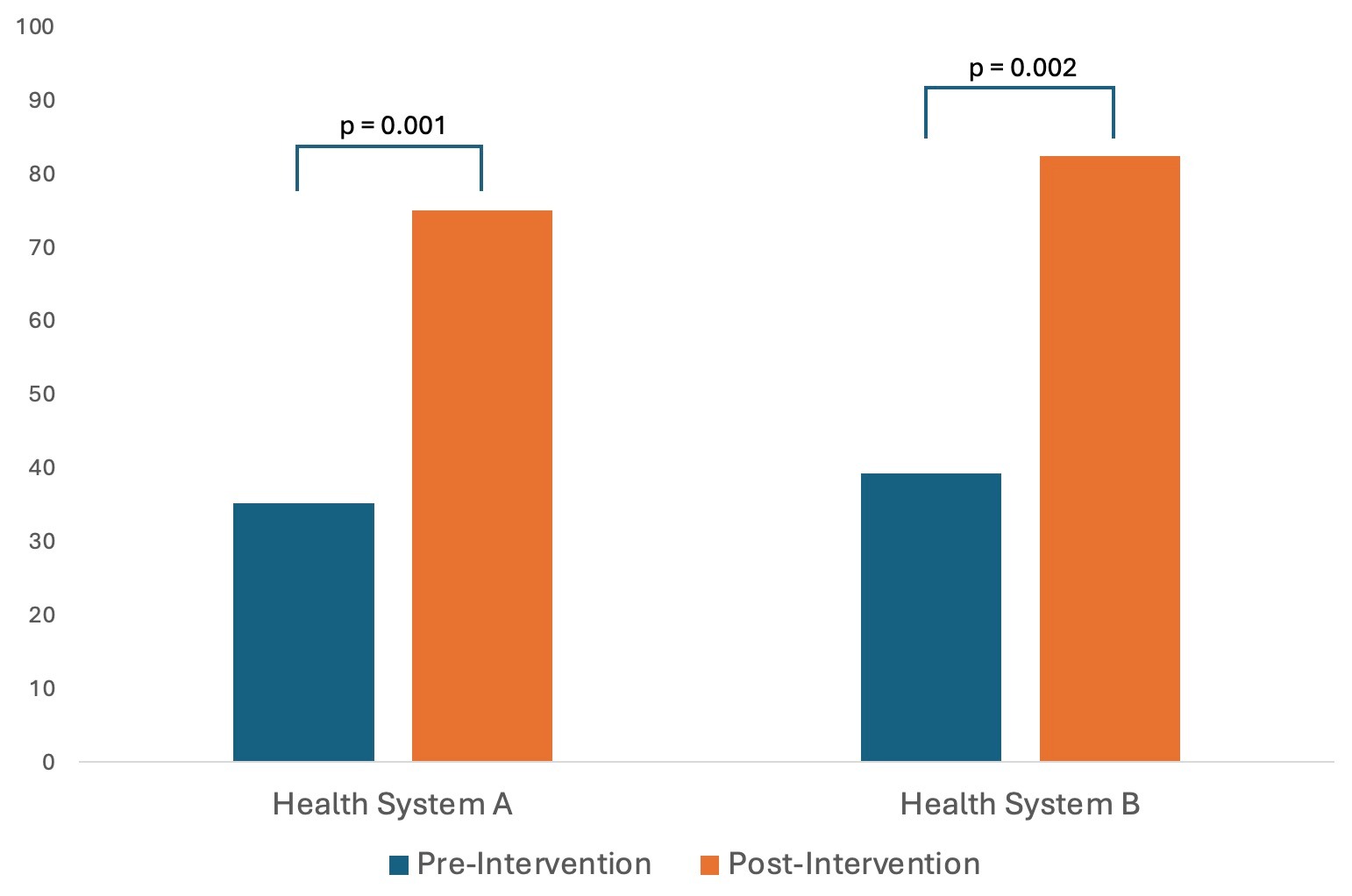
Results: There were 95 patients (71 pre- and 24 post-intervention) at Institution A and 78 patients (61 pre and 17 post) at Institution B. Patient characteristics and clinical findings were similar between groups (Table). Baseline FIBR was 35.2% and 39.4% at Institution A and B, respectively. There was a significant improvement in FIBR at both institutions, increasing to 75.0% (p=0.001) and 82.4% (p=0.002) at each center, respectively (Figure). The absolute difference was mostly due to implementation of standardized text, which was 37.5% at Institution A and 52.9% at Institution B. The proportion of patients prescribed a proton pump inhibitor post-EFI increased from 80.3% to 91.7% at Institution A (p=0.20) and 70.5% to 100.0% at Institution B (p=0.011). The proportion of patients diagnosed with EoE at time of EFI increased from 8.5% to 20.8% at Institution A (p=0.10) and 14.8% to 41.2% at Institution B (p=0.017).
Discussion: Implementation of a standardized protocol for EFI management led to an absolute increase in food impaction biopsy rate (FIBR) of 39.8% and 43.1% at two health systems. Post-EFI management also improved, suggesting this replicable behavioral “nudge” is a meaningful strategy to improve adherence to best practices in EoE care.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Walker D. Redd, MD1, Courtney Richman, MD2, Trevor Barlowe, MD1, Sabrina Layne, MD2, Angel Miro-Gonzalez, MD1, Nirmala Gonsalves, MD3, Evan S.. Dellon, MD, MPH, FACG1, David A. Leiman, MD, MSHP4. P3928 - Marked Improvement in Esophageal Food Impaction Biopsy Rate (FIBR) After Implementation of a Multicenter Behavioral Intervention, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of North Carolina at Chapel Hill School of Medicine, Chapel Hill, NC; 2Duke University School of Medicine, Durham, NC; 3Feinberg School of Medicine, Northwestern University, Chicago, IL; 4Duke University School of Medicine, Chapel Hill, NC
Introduction: Performing esophageal biopsies at the time of esophageal food impaction (EFI) is a quality indicator in eosinophilic esophagitis (EoE) but is infrequently performed leading to diagnostic delay. We aimed to determine whether a behavioral intervention could improve the food impaction biopsy rate (FIBR) and quality of EFI follow-up care.
Methods: We created a standardized electronic health record (EHR) protocol that could be embedded within the EFI treatment pathway. This algorithm was shared among clinicians and posted in the endoscopy units at four locations across two health systems. We obtained baseline FIBR performance rates among adults undergoing upper endoscopy from 7/1/2021-6/30/2023 and assessed post-intervention outcomes from 10/2/2023-4/2/2024. Patient demographics, clinical, procedural, and management details were extracted from the EHR. The primary outcome was the FIBR, defined as the proportion of patients with esophageal biopsies performed at time of endoscopy for EFI. Patients with impacted nonfood foreign bodies were excluded. Pre- and post-intervention data were compared using bivariate statistics. Data from each center were analyzed separately to assess for replicability of results.
Results: There were 95 patients (71 pre- and 24 post-intervention) at Institution A and 78 patients (61 pre and 17 post) at Institution B. Patient characteristics and clinical findings were similar between groups (Table). Baseline FIBR was 35.2% and 39.4% at Institution A and B, respectively. There was a significant improvement in FIBR at both institutions, increasing to 75.0% (p=0.001) and 82.4% (p=0.002) at each center, respectively (Figure). The absolute difference was mostly due to implementation of standardized text, which was 37.5% at Institution A and 52.9% at Institution B. The proportion of patients prescribed a proton pump inhibitor post-EFI increased from 80.3% to 91.7% at Institution A (p=0.20) and 70.5% to 100.0% at Institution B (p=0.011). The proportion of patients diagnosed with EoE at time of EFI increased from 8.5% to 20.8% at Institution A (p=0.10) and 14.8% to 41.2% at Institution B (p=0.017).
Discussion: Implementation of a standardized protocol for EFI management led to an absolute increase in food impaction biopsy rate (FIBR) of 39.8% and 43.1% at two health systems. Post-EFI management also improved, suggesting this replicable behavioral “nudge” is a meaningful strategy to improve adherence to best practices in EoE care.
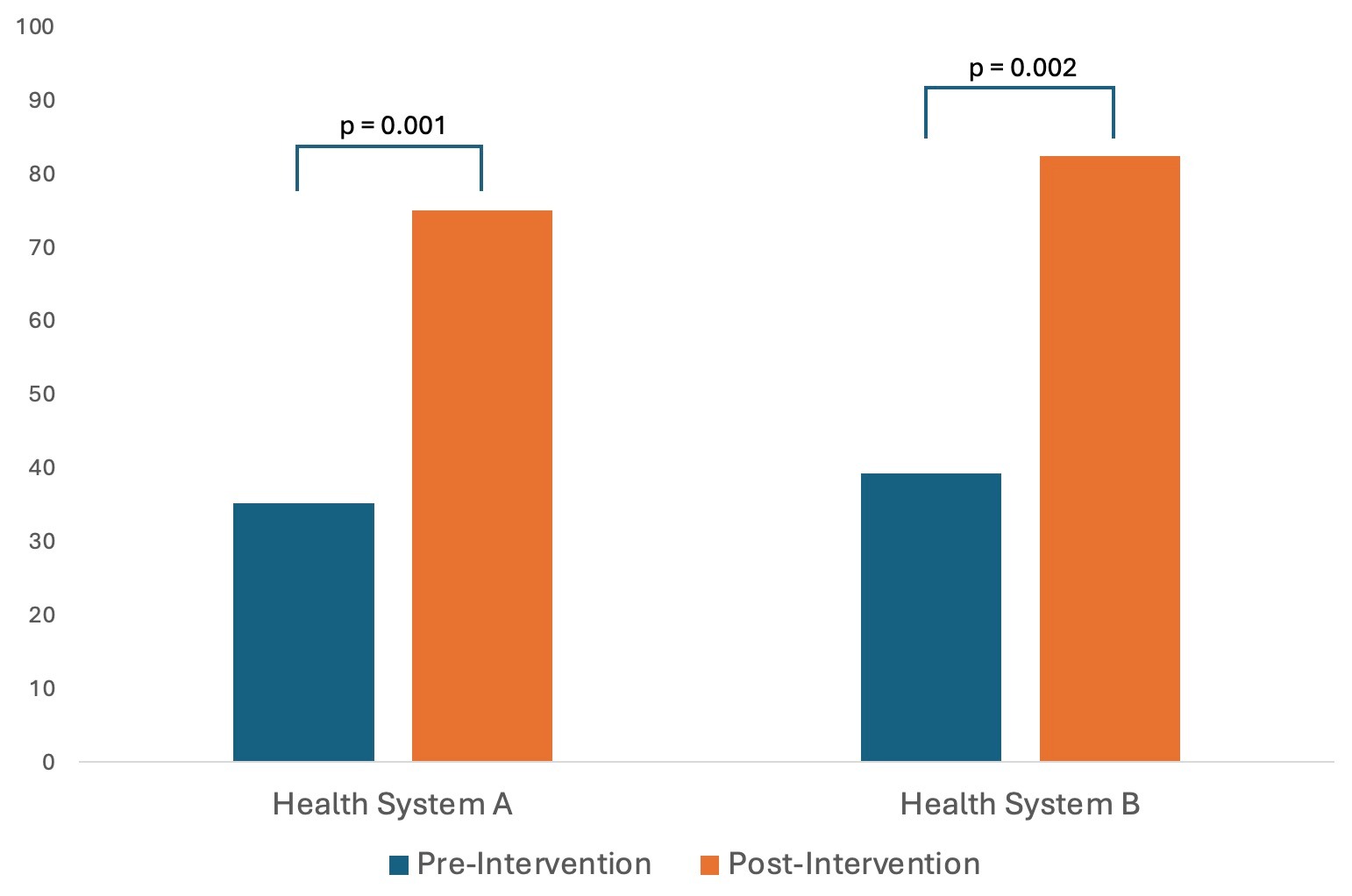
Figure: Figure. Food impaction biopsy rate (FIBR) Pre-Intervention and Post-Intervention
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Walker Redd indicated no relevant financial relationships.
Courtney Richman indicated no relevant financial relationships.
Trevor Barlowe indicated no relevant financial relationships.
Sabrina Layne indicated no relevant financial relationships.
Angel Miro-Gonzalez indicated no relevant financial relationships.
Nirmala Gonsalves indicated no relevant financial relationships.
Evan Dellon: Abbott – Consultant. AbbVie – Consultant. Adare/Ellodi – Consultant, Grant/Research Support. Aimmune – Consultant. Akesobio – Consultant. Alfasigma – Consultant. ALK – Consultant. Allakos – Consultant, Grant/Research Support. Amgen – Consultant. Aqilion – Consultant, Grant/Research Support. Arena/Pfizer – Consultant, Grant/Research Support. Aslan – Consultant. AstraZeneca – Consultant, Grant/Research Support. Avir – Consultant. Biorasi – Consultant. Calypso – Consultant. Celgene/Receptos/BMS – Consultant, Grant/Research Support. Celldex – Consultant. Dr. Falk Pharma – Consultant. Eli Lilly – Consultant. EsoCap – Consultant. Eupraxia – Consultant, Grant/Research Support. Ferring – Consultant, Grant/Research Support. GlaxoSmithKline – Consultant, Grant/Research Support. Gossamer Bio – Consultant. Holoclara – Consultant. Holoclara – Grant/Research Support. Invea – Consultant. Invea – Grant/Research Support. Knightpoint – Consultant. Landos – Consultant. LucidDx – Consultant. Meritage – Grant/Research Support. Miraca – Grant/Research Support. Morphic – Consultant. Nexstone Immunology/Uniquity – Consultant. Nutricia – Consultant, Grant/Research Support. Parexel/Calyx – Consultant. Phathom – Consultant. Regeneron Pharmaceuticals Inc. – Consultant, Grant/Research Support. Revolo – Consultant, Grant/Research Support. Robarts/Alimentiv – Consultant. Salix – Consultant. Sanofi – Consultant. Shire/Takeda – Consultant, Grant/Research Support. Target RWE – Consultant. Upstream Bio – Consultant.
David Leiman: Astra Zeneca – Consultant. Bristol Myers Squibb – Stock-publicly held company(excluding mutual/index funds). Merck – Consultant. Novo Nordisk – Consultant. Regeneron – Advisory Committee/Board Member. Sanofi – Advisory Committee/Board Member. TargetRWE – Advisor or Review Panel Member.
Walker D. Redd, MD1, Courtney Richman, MD2, Trevor Barlowe, MD1, Sabrina Layne, MD2, Angel Miro-Gonzalez, MD1, Nirmala Gonsalves, MD3, Evan S.. Dellon, MD, MPH, FACG1, David A. Leiman, MD, MSHP4. P3928 - Marked Improvement in Esophageal Food Impaction Biopsy Rate (FIBR) After Implementation of a Multicenter Behavioral Intervention, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
