Tuesday Poster Session
Category: Esophagus
P3946 - Reducing Proton Pump Inhibitor Overuse Through PPI De-Prescription: A Primary Care Quality Improvement Project
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- DZ
Duha Zaffar, MD
University of Maryland Medical Center
Baltimore, MD
Presenting Author(s)
Duha Zaffar, MD, Mohammad Hossain, MD, Jeffrey Gerbino, MD, Bruce D.. Greenwald, MD
University of Maryland Medical Center, Baltimore, MD
Introduction: Proton pump inhibitor (PPI) use is extremely common. Developed for the treatment and prevention of acid-mediated upper GI conditions, these agents are used increasingly for indications where benefit is less certain. PPI over-prescription imposes an economic cost and contributes to polypharmacy. In addition, PPI use has been increasingly linked to a number of adverse events. Therefore, de-prescribing of PPIs is an important strategy to lower pill burden while reducing real costs and theoretical risks.
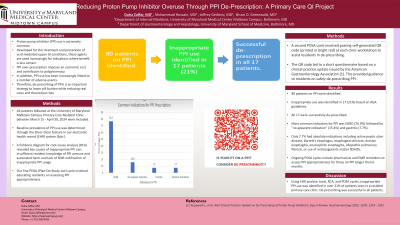
Methods: All patients followed at the University of Maryland Midtown Campus Primary Care Resident Clinic between March 15 - April 30, 2024 were included. Baseline prevalence of PPI use was determined through the Slicer-Dicer feature in our electronic health record (EHR) system (Epic). A fishbone diagram for root-cause analysis (RCA) revealed key causes of inappropriate PPI use: insufficient resident knowledge of PPI overuse and associated harm and lack of EMR notification of inappropriate PPI usage. Our first PDSA (Plan-Do-Study-Act) cycle involved educating residents on assessing PPI appropriateness. A second PDSA cycle involved pasting self-generated QR code (printed in bright red) at each clinic workstation to assist residents in de-prescribing. The QR code led to a short questionnaire based on a clinical practice update issued by the American Gastroenterology Association (1). This provided guidance to residents on safely de-prescribing PPI.
Results: 80 patients on PPI were identified. Inappropriate use was identified in 17 (21%) based on AGA guidelines. All 17 were successfully de-prescribed. Most common indication for PPI was GERD (76.9%) followed by "no apparent indication" (15.4%) and gastritis (7.7%). Only 7.7% had absolute indications including active peptic ulcer disease, Barrett’s esophagus, esophageal stricture, erosive esophagitis, eosinophilic esophagitis, idiopathic pulmonary fibrosis, or use of anticoagulants and/or NSAIDs. Ongoing PDSA cycles include pharmacists and EMR reminders to assess PPI appropriateness for those on PPI longer than 6 months.
Discussion: Using EHR analytic tools, RCA, and PDSA cycles, inappropriate PPI use was identified in over 21% of patients seen in a resident primary care clinic. De-prescribing was successful in all patients.
(1) Targownik L, et al. AGA Clinical Practice Update on De-Prescribing of Proton Pump Inhibitors: Expert Review. Gastroenterology 2022; 12(4): 1334 - 1342
Disclosures:
Duha Zaffar, MD, Mohammad Hossain, MD, Jeffrey Gerbino, MD, Bruce D.. Greenwald, MD. P3946 - Reducing Proton Pump Inhibitor Overuse Through PPI De-Prescription: A Primary Care Quality Improvement Project, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
University of Maryland Medical Center, Baltimore, MD
Introduction: Proton pump inhibitor (PPI) use is extremely common. Developed for the treatment and prevention of acid-mediated upper GI conditions, these agents are used increasingly for indications where benefit is less certain. PPI over-prescription imposes an economic cost and contributes to polypharmacy. In addition, PPI use has been increasingly linked to a number of adverse events. Therefore, de-prescribing of PPIs is an important strategy to lower pill burden while reducing real costs and theoretical risks.
Methods: All patients followed at the University of Maryland Midtown Campus Primary Care Resident Clinic between March 15 - April 30, 2024 were included. Baseline prevalence of PPI use was determined through the Slicer-Dicer feature in our electronic health record (EHR) system (Epic). A fishbone diagram for root-cause analysis (RCA) revealed key causes of inappropriate PPI use: insufficient resident knowledge of PPI overuse and associated harm and lack of EMR notification of inappropriate PPI usage. Our first PDSA (Plan-Do-Study-Act) cycle involved educating residents on assessing PPI appropriateness. A second PDSA cycle involved pasting self-generated QR code (printed in bright red) at each clinic workstation to assist residents in de-prescribing. The QR code led to a short questionnaire based on a clinical practice update issued by the American Gastroenterology Association (1). This provided guidance to residents on safely de-prescribing PPI.
Results: 80 patients on PPI were identified. Inappropriate use was identified in 17 (21%) based on AGA guidelines. All 17 were successfully de-prescribed. Most common indication for PPI was GERD (76.9%) followed by "no apparent indication" (15.4%) and gastritis (7.7%). Only 7.7% had absolute indications including active peptic ulcer disease, Barrett’s esophagus, esophageal stricture, erosive esophagitis, eosinophilic esophagitis, idiopathic pulmonary fibrosis, or use of anticoagulants and/or NSAIDs. Ongoing PDSA cycles include pharmacists and EMR reminders to assess PPI appropriateness for those on PPI longer than 6 months.
Discussion: Using EHR analytic tools, RCA, and PDSA cycles, inappropriate PPI use was identified in over 21% of patients seen in a resident primary care clinic. De-prescribing was successful in all patients.
(1) Targownik L, et al. AGA Clinical Practice Update on De-Prescribing of Proton Pump Inhibitors: Expert Review. Gastroenterology 2022; 12(4): 1334 - 1342
Disclosures:
Duha Zaffar indicated no relevant financial relationships.
Mohammad Hossain indicated no relevant financial relationships.
Jeffrey Gerbino indicated no relevant financial relationships.
Bruce Greenwald indicated no relevant financial relationships.
Duha Zaffar, MD, Mohammad Hossain, MD, Jeffrey Gerbino, MD, Bruce D.. Greenwald, MD. P3946 - Reducing Proton Pump Inhibitor Overuse Through PPI De-Prescription: A Primary Care Quality Improvement Project, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
