Tuesday Poster Session
Category: Esophagus
P3951 - Diverse Presentations and Diagnostic Challenges in Cytomegalovirus (CMV) Esophagitis: A Case Series
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E

Aalesh Shah, MBBS
Smt. NHL Municipal Medical College
Ahmedabad, Gujarat, India
Presenting Author(s)
Aalesh Shah, MBBS1,Yug Patel, MBBS1, Vishal Beriwala, MBBS, MD2
1Smt. NHL Municipal Medical College, Ahmedabad, Gujarat, India; 2SVP Institute of Medical Sciences and Research, Ahmedabad, Gujarat, India
Introduction: CMV esophagitis, the second most common CMV gastrointestinal infection after colitis, primarily affects immunocompromised individuals but is being increasingly recognized in immunocompetent patients. Diagnosis depends on histological identification of CMV inclusion bodies, with macroscopic endoscopic findings often revealing characteristic ulcers.
Case Description/Methods: 1. A 70-year-old male with a history of tobacco use presented with progressive dysphagia, vomiting, and significant weight loss. Histology and immunohistochemistry confirmed CMV esophagitis.
2. A female with no comorbidities reported fever, epigastric pain, regurgitation, and retrosternal pain for 5-7 days. Endoscopic biopsy showed ulcerated squamous epithelium and CMV inclusions, confirming CMV esophagitis.
3. A 57-year-old male with Neuromyelitis Optica on immunosuppressive therapy and a history of pulmonary tuberculosis presented with hematemesis. Endoscopy revealed severe erosive esophagitis and histology confirmed CMV infection. Treatment with ganciclovir and valganciclovir was administered.
4. A 70-year-old male with no comorbidities, presented with retrosternal chest pain and hematemesis. He had endoscopic findings of circumferentially inflamed esophagus. Histological examination confirmed CMV esophagitis and valganciclovir treatment was prescribed.
5. A 67-year-old male with chronic alcoholism and tobacco use presented with hematemesis and vomiting. Endoscopy showed serpiginous ulcerations, and histology confirmed CMV esophagitis. Treatment included valganciclovir.
6. A 50-year-old female with throat pain, dysphagia, and earache was diagnosed with CMV esophagitis and mild inactive gastritis. Management included intravenous ganciclovir and supportive care.
7. A patient with HIV/AIDS presented with gastrointestinal symptoms typical of CMV esophagitis. Histological examination confirmed the diagnosis and antiviral treatment was initiated.
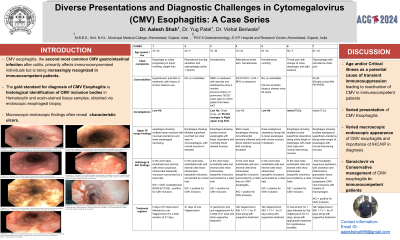
Discussion: Out of the 7 cases, two patients had conditions potentially increasing their risk of a symptomatic CMV infection, however, five patients had no classical significant risk factors predisposing them to CMV esophagitis. Endoscopic findings varied, particularly overlapping with HSV esophagitis, with some patients displaying classical linear ulcers and others showing atypical patterns. All the patients were treated with antivirals in the form of either IV Ganciclovir or Oral Valganciclovir in appropriate doses, following which patients showed clinical improvement.

Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Aalesh Shah, MBBS1, Yug Patel, MBBS1, Vishal Beriwala, MBBS, MD2. P3951 - Diverse Presentations and Diagnostic Challenges in Cytomegalovirus (CMV) Esophagitis: A Case Series, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Smt. NHL Municipal Medical College, Ahmedabad, Gujarat, India; 2SVP Institute of Medical Sciences and Research, Ahmedabad, Gujarat, India
Introduction: CMV esophagitis, the second most common CMV gastrointestinal infection after colitis, primarily affects immunocompromised individuals but is being increasingly recognized in immunocompetent patients. Diagnosis depends on histological identification of CMV inclusion bodies, with macroscopic endoscopic findings often revealing characteristic ulcers.
Case Description/Methods: 1. A 70-year-old male with a history of tobacco use presented with progressive dysphagia, vomiting, and significant weight loss. Histology and immunohistochemistry confirmed CMV esophagitis.
2. A female with no comorbidities reported fever, epigastric pain, regurgitation, and retrosternal pain for 5-7 days. Endoscopic biopsy showed ulcerated squamous epithelium and CMV inclusions, confirming CMV esophagitis.
3. A 57-year-old male with Neuromyelitis Optica on immunosuppressive therapy and a history of pulmonary tuberculosis presented with hematemesis. Endoscopy revealed severe erosive esophagitis and histology confirmed CMV infection. Treatment with ganciclovir and valganciclovir was administered.
4. A 70-year-old male with no comorbidities, presented with retrosternal chest pain and hematemesis. He had endoscopic findings of circumferentially inflamed esophagus. Histological examination confirmed CMV esophagitis and valganciclovir treatment was prescribed.
5. A 67-year-old male with chronic alcoholism and tobacco use presented with hematemesis and vomiting. Endoscopy showed serpiginous ulcerations, and histology confirmed CMV esophagitis. Treatment included valganciclovir.
6. A 50-year-old female with throat pain, dysphagia, and earache was diagnosed with CMV esophagitis and mild inactive gastritis. Management included intravenous ganciclovir and supportive care.
7. A patient with HIV/AIDS presented with gastrointestinal symptoms typical of CMV esophagitis. Histological examination confirmed the diagnosis and antiviral treatment was initiated.
Discussion: Out of the 7 cases, two patients had conditions potentially increasing their risk of a symptomatic CMV infection, however, five patients had no classical significant risk factors predisposing them to CMV esophagitis. Endoscopic findings varied, particularly overlapping with HSV esophagitis, with some patients displaying classical linear ulcers and others showing atypical patterns. All the patients were treated with antivirals in the form of either IV Ganciclovir or Oral Valganciclovir in appropriate doses, following which patients showed clinical improvement.

Figure: Endoscopic images showing the different types of lesions seen in the patients of CMV Esophagitis
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Aalesh Shah indicated no relevant financial relationships.
Yug Patel indicated no relevant financial relationships.
Vishal Beriwala indicated no relevant financial relationships.
Aalesh Shah, MBBS1, Yug Patel, MBBS1, Vishal Beriwala, MBBS, MD2. P3951 - Diverse Presentations and Diagnostic Challenges in Cytomegalovirus (CMV) Esophagitis: A Case Series, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
