Tuesday Poster Session
Category: Esophagus
P3957 - Dysphagia Aortica in an Elderly Patient: A Diagnostic and Therapeutic Challenge for Endoscopists
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Laura Miranda, MD
Broward Health North
Pompano Beach, FL
Presenting Author(s)
Laura Miranda, MD1, Keshavi Mahesh, MD1, Gautam Anand, MD2, Aryama Sharma, MD2
1Broward Health North, Pompano Beach, FL; 2Broward Health North, Fort Lauderdale, FL
Introduction: Dysphagia aortica (DA) is a rare condition caused by extrinsic compression of the esophagus by an ectatic, tortuous, or aneurysmatic aorta. Due to limited data, its prevalence and incidence rates remain unknown. Dysphagia, however, affects up to 33% of older adults and can lead to malnutrition, aspiration pneumonia, airway obstruction, or death. This case report highlights the challenges faced by endoscopists in diagnosing and managing DA, emphasizing the importance of early recognition and cautious endoscopic evaluation, given its high mortality rate.
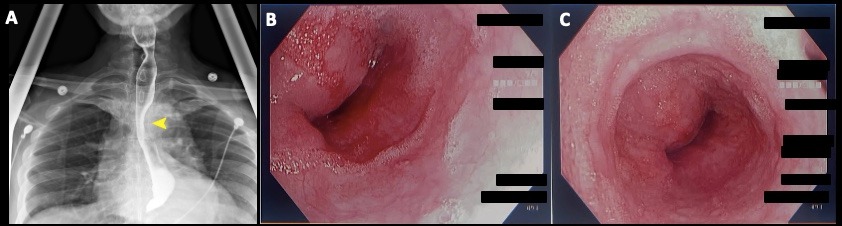
Case Description/Methods: An 80-year-old male presents with a 2-month history of generalized weakness, dry cough, dysphagia to solids, and a globus sensation. He endorses a 40-lb weight loss and poor oral intake. His medical history is relevant for ESRD on peritoneal dialysis and an open repair of an abdominal aortic aneurysm 5 years prior. Upon arrival, vital signs were stable. Physical exam revealed a PD catheter in place with a clean site and no surrounding erythema, tenderness or discharge. No other clinical findings were noted. Laboratory tests were notable for potassium 3.1, magnesium 1.1, serum creatinine 9.9, and BUN 43. Barium esophagram showed mass effect on the distal esophagus with preserved motility and a patent GE junction. CTA of the chest with contrast demonstrated a 6 cm descending TAA with a mixed atherosclerotic plaque eccentrically along the wall. An upper endoscopy showed extrinsic pulsatile compression of the distal esophagus at 22 cm from incisors. A decision was made to proceed with the surgical repair of his large TAA, which subsequently relieved his symptoms.
Discussion: DA should be considered in elderly patients with unexplained difficulty swallowing, especially those with known aortic pathology. It presents a unique challenge for endoscopists due to the anatomical distortion of the esophagus, risk of wall injury or perforation, limited visualization, and technical difficulties. Ruptured aortic aneurysms and dissections lead to approximately 30,000 deaths per year in the United States, with few cases reportedly associated with endoscopic evaluations, particularly those complicated by aortoesophageal fistulas. Prompt diagnosis and careful endoscopic evaluation are crucial to ensure patient safety and improve outcomes in this setting. Consideration should be given to using endoscopic ultrasound (EUS) to readily identify aortic aneurysms and their relationship with the esophagus.
Disclosures:
Laura Miranda, MD1, Keshavi Mahesh, MD1, Gautam Anand, MD2, Aryama Sharma, MD2. P3957 - Dysphagia Aortica in an Elderly Patient: A Diagnostic and Therapeutic Challenge for Endoscopists, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Broward Health North, Pompano Beach, FL; 2Broward Health North, Fort Lauderdale, FL
Introduction: Dysphagia aortica (DA) is a rare condition caused by extrinsic compression of the esophagus by an ectatic, tortuous, or aneurysmatic aorta. Due to limited data, its prevalence and incidence rates remain unknown. Dysphagia, however, affects up to 33% of older adults and can lead to malnutrition, aspiration pneumonia, airway obstruction, or death. This case report highlights the challenges faced by endoscopists in diagnosing and managing DA, emphasizing the importance of early recognition and cautious endoscopic evaluation, given its high mortality rate.
Case Description/Methods: An 80-year-old male presents with a 2-month history of generalized weakness, dry cough, dysphagia to solids, and a globus sensation. He endorses a 40-lb weight loss and poor oral intake. His medical history is relevant for ESRD on peritoneal dialysis and an open repair of an abdominal aortic aneurysm 5 years prior. Upon arrival, vital signs were stable. Physical exam revealed a PD catheter in place with a clean site and no surrounding erythema, tenderness or discharge. No other clinical findings were noted. Laboratory tests were notable for potassium 3.1, magnesium 1.1, serum creatinine 9.9, and BUN 43. Barium esophagram showed mass effect on the distal esophagus with preserved motility and a patent GE junction. CTA of the chest with contrast demonstrated a 6 cm descending TAA with a mixed atherosclerotic plaque eccentrically along the wall. An upper endoscopy showed extrinsic pulsatile compression of the distal esophagus at 22 cm from incisors. A decision was made to proceed with the surgical repair of his large TAA, which subsequently relieved his symptoms.
Discussion: DA should be considered in elderly patients with unexplained difficulty swallowing, especially those with known aortic pathology. It presents a unique challenge for endoscopists due to the anatomical distortion of the esophagus, risk of wall injury or perforation, limited visualization, and technical difficulties. Ruptured aortic aneurysms and dissections lead to approximately 30,000 deaths per year in the United States, with few cases reportedly associated with endoscopic evaluations, particularly those complicated by aortoesophageal fistulas. Prompt diagnosis and careful endoscopic evaluation are crucial to ensure patient safety and improve outcomes in this setting. Consideration should be given to using endoscopic ultrasound (EUS) to readily identify aortic aneurysms and their relationship with the esophagus.
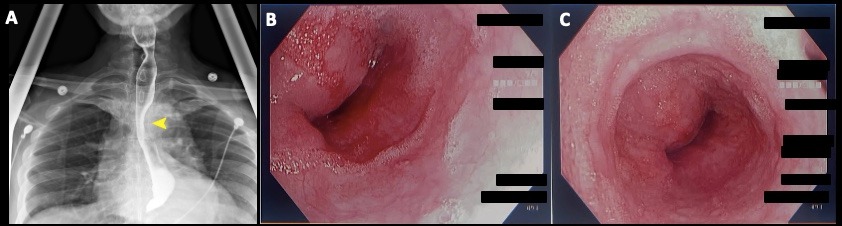
Figure: (A) Barium esophagram showing stenosis of the distal esophagus at the level of the origin of the descending aorta (yellow arrowhead), as well as a tortuous appearance. (B,C) Endoscopic images demonstrating extrinsic compression of the distal esophagus due to mass effect at 22 cm from incisors.
Disclosures:
Laura Miranda indicated no relevant financial relationships.
Keshavi Mahesh indicated no relevant financial relationships.
Gautam Anand indicated no relevant financial relationships.
Aryama Sharma indicated no relevant financial relationships.
Laura Miranda, MD1, Keshavi Mahesh, MD1, Gautam Anand, MD2, Aryama Sharma, MD2. P3957 - Dysphagia Aortica in an Elderly Patient: A Diagnostic and Therapeutic Challenge for Endoscopists, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

