Tuesday Poster Session
Category: Esophagus
P3959 - Metastatic Esophageal Adenocarcinoma in a Healthy 19-Year-Old Female
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Himaben Gohil, DO
University of Buffalo
Buffalo, NY
Presenting Author(s)
Award: Presidential Poster Award
Himaben Gohil, DO1, Austin Knorz, BS1, Jason Edwards, MD2, Clive J. Miranda, DO, MSc3, Thomas Mahl, MD2
1University of Buffalo, Buffalo, NY; 2University at Buffalo, Buffalo, NY; 3CHI Health Creighton University Medical Center, Omaha, NE
Introduction: Esophageal adenocarcinoma (EAC) is uncommon in individuals less than 50 years old because it is assumed that EAC develops following years of gastroesophageal reflux disease (GERD) leading to intestinal metaplasia (IM) followed by Barrett’s esophagus (BE) and ultimately EAC. Here we present a case of a 19-year-old female with no history of heartburn who was diagnosed with esophageal adenocarcinoma with metastasis to lymph nodes and bone.
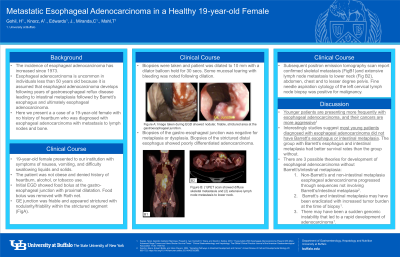
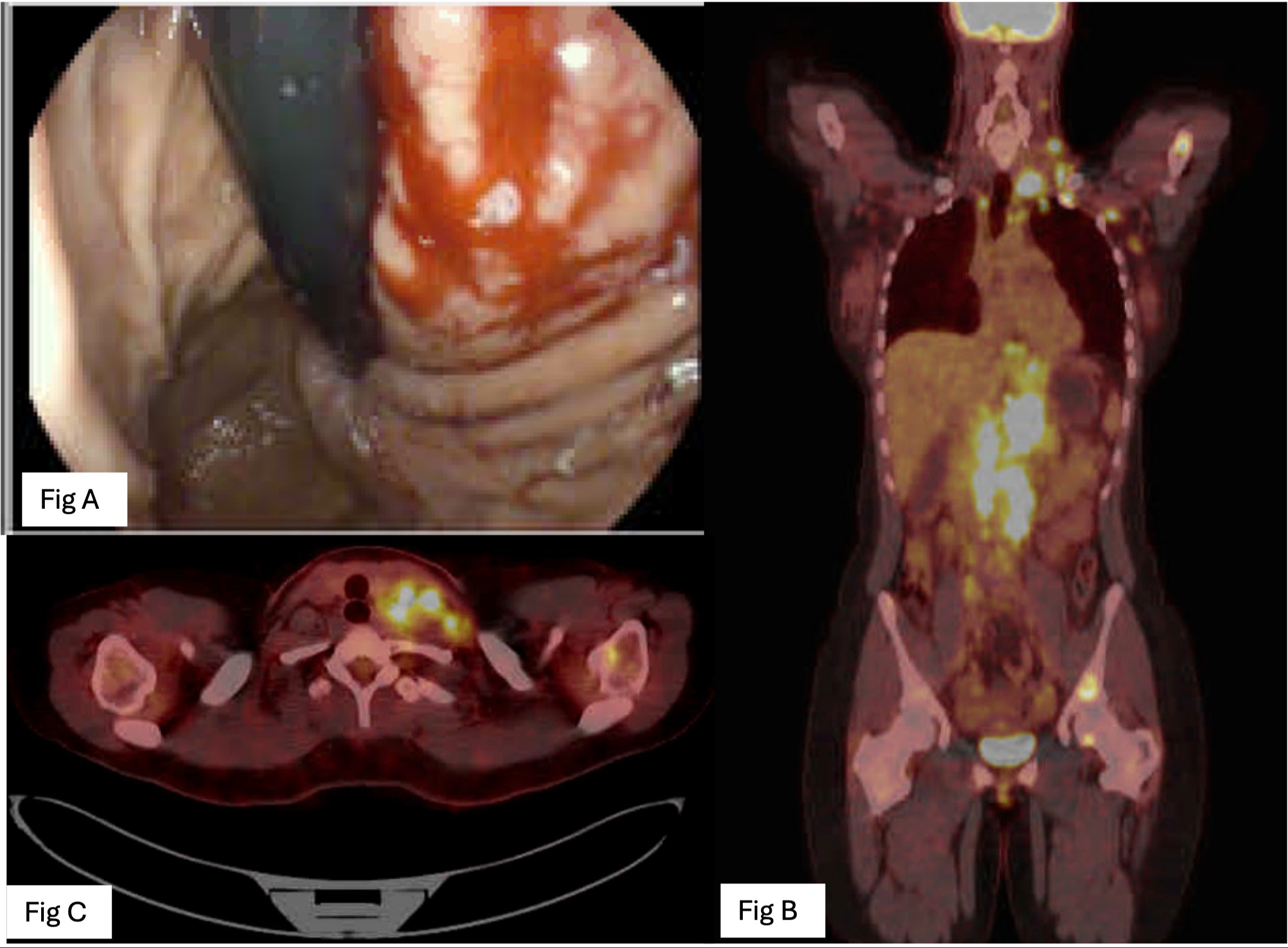
Case Description/Methods: A 19-year-old female presented to our institution with symptoms of nausea, vomiting, and progressive dysphagia for a month. The patient was not obese and denied history of heartburn, alcohol, or tobacco use. An esophagogastroduodenoscopy (EGD) showed a nodular, friable, strictured area at the gastroesophageal junction (GEJ) (Fig A). Biopsies of the GEJ were negative for metaplasia and dysplasia. Biopsies of the abnormal appearing area confirmed poorly differentiated adenocarcinoma. Biopsies of the adjacent seemingly uninvolved mucosa did not show metaplasia. Subsequent positron emission tomography scan confirmed skeletal metastasis (Fig B) and extensive lymph node metastasis to lower neck (Fig C), abdomen, chest and to lesser degree pelvis. Fine needle aspiration cytology of the left cervical lymph node biopsy was positive for malignancy. The patient was eventually started on a palliative chemotherapy regimen.
Discussion: A recent large center retrospective report by Sawas et al., 2019 suggested that younger patients are presenting more frequently with EAC, and their cancers are more aggressive. Interestingly a single center study found that most young patients diagnosed with EAC did not have BE or IM. Similar to our patient who’s normal appearing GEJ biopsy was negative for metaplasia or dysplasia. Furthermore, the group with BE and IM had better survival rates than the group without BE and IM. The authors suggested three possibilities for development of EAC without BE/IM, first being that non-BE and non-IM EAC progressed through sequences not involving BE/IM. Secondly, BE and IM may have been eradicated with increased tumor burden at the time of biopsy. Lastly, there may have been a sudden genomic instability that led to a rapid development of adenocarcinoma. Due to the devastating consequences of EAC presenting at a later stage in young adults it is critical to further study the etiology involved in the development of EAC in the young population.
Disclosures:
Himaben Gohil, DO1, Austin Knorz, BS1, Jason Edwards, MD2, Clive J. Miranda, DO, MSc3, Thomas Mahl, MD2. P3959 - Metastatic Esophageal Adenocarcinoma in a Healthy 19-Year-Old Female, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Himaben Gohil, DO1, Austin Knorz, BS1, Jason Edwards, MD2, Clive J. Miranda, DO, MSc3, Thomas Mahl, MD2
1University of Buffalo, Buffalo, NY; 2University at Buffalo, Buffalo, NY; 3CHI Health Creighton University Medical Center, Omaha, NE
Introduction: Esophageal adenocarcinoma (EAC) is uncommon in individuals less than 50 years old because it is assumed that EAC develops following years of gastroesophageal reflux disease (GERD) leading to intestinal metaplasia (IM) followed by Barrett’s esophagus (BE) and ultimately EAC. Here we present a case of a 19-year-old female with no history of heartburn who was diagnosed with esophageal adenocarcinoma with metastasis to lymph nodes and bone.
Case Description/Methods: A 19-year-old female presented to our institution with symptoms of nausea, vomiting, and progressive dysphagia for a month. The patient was not obese and denied history of heartburn, alcohol, or tobacco use. An esophagogastroduodenoscopy (EGD) showed a nodular, friable, strictured area at the gastroesophageal junction (GEJ) (Fig A). Biopsies of the GEJ were negative for metaplasia and dysplasia. Biopsies of the abnormal appearing area confirmed poorly differentiated adenocarcinoma. Biopsies of the adjacent seemingly uninvolved mucosa did not show metaplasia. Subsequent positron emission tomography scan confirmed skeletal metastasis (Fig B) and extensive lymph node metastasis to lower neck (Fig C), abdomen, chest and to lesser degree pelvis. Fine needle aspiration cytology of the left cervical lymph node biopsy was positive for malignancy. The patient was eventually started on a palliative chemotherapy regimen.
Discussion: A recent large center retrospective report by Sawas et al., 2019 suggested that younger patients are presenting more frequently with EAC, and their cancers are more aggressive. Interestingly a single center study found that most young patients diagnosed with EAC did not have BE or IM. Similar to our patient who’s normal appearing GEJ biopsy was negative for metaplasia or dysplasia. Furthermore, the group with BE and IM had better survival rates than the group without BE and IM. The authors suggested three possibilities for development of EAC without BE/IM, first being that non-BE and non-IM EAC progressed through sequences not involving BE/IM. Secondly, BE and IM may have been eradicated with increased tumor burden at the time of biopsy. Lastly, there may have been a sudden genomic instability that led to a rapid development of adenocarcinoma. Due to the devastating consequences of EAC presenting at a later stage in young adults it is critical to further study the etiology involved in the development of EAC in the young population.
Figure: Figure: (A) Image taken during EGD showed nodular, friable, strictured area at the gastroesophageal junction. (B) PET scan showed diffuse skeletal metastasis and (C) extensive lymph node metastasis to lower neck.
Disclosures:
Himaben Gohil indicated no relevant financial relationships.
Austin Knorz indicated no relevant financial relationships.
Jason Edwards indicated no relevant financial relationships.
Clive Miranda indicated no relevant financial relationships.
Thomas Mahl indicated no relevant financial relationships.
Himaben Gohil, DO1, Austin Knorz, BS1, Jason Edwards, MD2, Clive J. Miranda, DO, MSc3, Thomas Mahl, MD2. P3959 - Metastatic Esophageal Adenocarcinoma in a Healthy 19-Year-Old Female, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

