Tuesday Poster Session
Category: Esophagus
P3963 - Acute Esophageal Necrosis: A Case Report on Management and Complications
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- SF
Sarah Fitzpatrick, MD
Madigan Army Medical Center
Olympia, WA
Presenting Author(s)
Sarah Fitzpatrick, MD
Madigan Army Medical Center, Olympia, WA
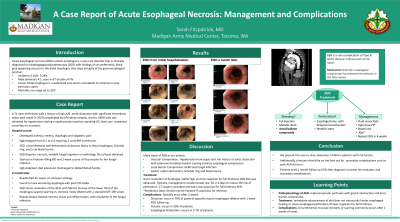
Introduction: Acute esophageal necrosis (AEN) or commonly termed black esophagus is a rare disorder that is clinically diagnosed on esophagogastroduodenoscopy (EGD) with characteristic findings of circumferential, black appearing mucosa to the distal esophagus that stops abruptly at the GEJ. AEN typically presents in men four times more often in females. This case of AEN likely occurred given her vascular compromise from a Type A aortic dissection, systemic infection, possible local fungal infection with esophageal barrier compromise from a large hiatal hernia. The case demonstrates that immediate advancement of diet does not necessarily hinder esophageal healing. Additionally, it divulges secondary complications of AEN such as stenosis.
Case Description/Methods: A 71-year-old female with a history significant for type A aortic dissection complicated by left kidney compromise admitted for urosepsis who underwent placement of a nephrostomy tube. Her hospital course was complicated by melena with anemia (Hgb-drop from 8.1 to 6.4) requiring transfusion. She endorsed new intermittent solid food and pill dysphagia which coincided with the onset of melena. EGD was performed demonstrating a sharp demarcation from normal appearing esophagus to violaceous dusky and even black appearing esophagus with a 6cm hiatal hernia and nonobstructive Schatzki ring. Biopsy confirmed AEN solidifying the diagnosis. Notably there were fungal elements on biopsy. She was started on Protonix 40mg twice a day, antifungals and placed on a mechanical soft diet. Her hemoglobin stabilized and she was discharged home. A month later, the patient was readmitted and found to have worsening dysphagia with progressive intolerance to solids since her last discharge with poor oral intake and weight loss. EGD was repeated and showed gross resolution of the AEN, with fibrotic mucosa of the lower third of the esophagus and intrinsic moderate circumferential scarring which was easily dilated with a standard GIF-190 scope. Repeat biopsies showed necrotic tissue and inflammation, but with resolution of the fungal infection.
Discussion: This case illustrates a typical presentation of AEN in a female most likely due to a hypotensive state from urosepsis along with gross resolution of her AEN several weeks later with medical/conservative management, complicated by esophageal stenosis. Her hiatal hernia and Schatzki ring most likely aided in esophageal barrier compromise. We present this case to raise awareness of AEN and to highlight post-AEN stricture.
Disclosures:
Sarah Fitzpatrick, MD. P3963 - Acute Esophageal Necrosis: A Case Report on Management and Complications, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Madigan Army Medical Center, Olympia, WA
Introduction: Acute esophageal necrosis (AEN) or commonly termed black esophagus is a rare disorder that is clinically diagnosed on esophagogastroduodenoscopy (EGD) with characteristic findings of circumferential, black appearing mucosa to the distal esophagus that stops abruptly at the GEJ. AEN typically presents in men four times more often in females. This case of AEN likely occurred given her vascular compromise from a Type A aortic dissection, systemic infection, possible local fungal infection with esophageal barrier compromise from a large hiatal hernia. The case demonstrates that immediate advancement of diet does not necessarily hinder esophageal healing. Additionally, it divulges secondary complications of AEN such as stenosis.
Case Description/Methods: A 71-year-old female with a history significant for type A aortic dissection complicated by left kidney compromise admitted for urosepsis who underwent placement of a nephrostomy tube. Her hospital course was complicated by melena with anemia (Hgb-drop from 8.1 to 6.4) requiring transfusion. She endorsed new intermittent solid food and pill dysphagia which coincided with the onset of melena. EGD was performed demonstrating a sharp demarcation from normal appearing esophagus to violaceous dusky and even black appearing esophagus with a 6cm hiatal hernia and nonobstructive Schatzki ring. Biopsy confirmed AEN solidifying the diagnosis. Notably there were fungal elements on biopsy. She was started on Protonix 40mg twice a day, antifungals and placed on a mechanical soft diet. Her hemoglobin stabilized and she was discharged home. A month later, the patient was readmitted and found to have worsening dysphagia with progressive intolerance to solids since her last discharge with poor oral intake and weight loss. EGD was repeated and showed gross resolution of the AEN, with fibrotic mucosa of the lower third of the esophagus and intrinsic moderate circumferential scarring which was easily dilated with a standard GIF-190 scope. Repeat biopsies showed necrotic tissue and inflammation, but with resolution of the fungal infection.
Discussion: This case illustrates a typical presentation of AEN in a female most likely due to a hypotensive state from urosepsis along with gross resolution of her AEN several weeks later with medical/conservative management, complicated by esophageal stenosis. Her hiatal hernia and Schatzki ring most likely aided in esophageal barrier compromise. We present this case to raise awareness of AEN and to highlight post-AEN stricture.
Disclosures:
Sarah Fitzpatrick indicated no relevant financial relationships.
Sarah Fitzpatrick, MD. P3963 - Acute Esophageal Necrosis: A Case Report on Management and Complications, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
