Tuesday Poster Session
Category: Endoscopy Video Forum
P3880 - A Maddening Migration of an Esophageal Stent
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- CE
Charles D. Evers, III, MD, MBA
University of Alabama at Birmingham Heersink School of Medicine
Homewood, AL
Presenting Author(s)
Charles D. Evers, MD, MBA1, Thomas Ruli, MD2, John A. Cooper, MD3, Mahmoud Aryan, MD3, Ethan D. Pollack, MS, MD3, Ramzi Mulki, MD4, Kabir Baig Kyanum, MD4, Sergio Sanchez-Luna, MD4, Ali Ahmed, MD4, Shajan Peter, MD4
1University of Alabama at Birmingham Heersink School of Medicine, Homewood, AL; 2University of Alabama at Birmingham, Birmingham, AL; 3University of Alabama at Birmingham Heersink School of Medicine, Birmingham, AL; 4Basil I. Hirschowitz Endoscopic Center of Excellence, The University of Alabama at Birmingham Heersink School of Medicine, Birmingham, AL
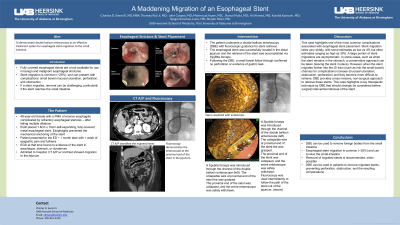
Introduction: Fully covered stents are a tool for the endoscopist in the management of benign and malignant strictures of the esophagus. Nevertheless, they come with potential risks to the patient, such as stent migration and related complications. Retrieval of these stents can be challenging, especially if they reach the small bowel. Here, we present a case of a migrated esophageal stent to the jejunum which was successfully retrieved via double-balloon enteroscopy (DBE) with fluoroscopic guidance.
Case Description/Methods: The patient is a 48-year-old woman with a history of ulcerative esophagitis complicated by esophageal stricture. The patient originally underwent an esophagogastroduodenoscopy (EGD) in which a 1.8x10 cm fully covered, self-expandable stent was placed at the site of the esophageal stricture. One month later, before a planned follow up EGD, she reported a week-long history of upper abdominal pain and fullness. EGD demonstrated that the previously deployed stent was absent from the esophagus; further investigation of the patient's stomach, duodenum, and proximal portion of the jejunum did not show the stent, either. A computed tomography abdomen and pelvis with contrast demonstrated the migrated esophageal stent in the mid-jejunum with local inflammation. The patient then underwent a DBE with fluoroscopic guidance for stent retrieval. The esophageal stent was successfully located in the distal jejunum and the retrieval of the stent was accomplished via SpyBite forceps [Please refer to video for procedure]. Following the DBE, a small bowel follow through confirmed no perforation or evidence of gastric leak.
Discussion: This case highlights one of the most common complications associated with esophageal stent placement. Stent migration rates vary widely, with some estimates as low as 4% but other estimates ranging as high as 30%. A large portion of stent migrations are asymptomatic. In some cases, such as when the stent remains in the stomach, a conservative approach can be taken (leaving the stent in place). However, when the stent migrates further into the gastrointestinal tract (such as into the small bowel), chances for complications increase (mucosal ulceration, obstruction, perforation) and they become more difficult to retrieve. DBE provides a less invasive, non-surgical approach to retrieve these stents. This case highlights a key therapeutic technique by DBE that should strongly be considered before surgical intervention/retrieval of the stent.
Disclosures:
Charles D. Evers, MD, MBA1, Thomas Ruli, MD2, John A. Cooper, MD3, Mahmoud Aryan, MD3, Ethan D. Pollack, MS, MD3, Ramzi Mulki, MD4, Kabir Baig Kyanum, MD4, Sergio Sanchez-Luna, MD4, Ali Ahmed, MD4, Shajan Peter, MD4. P3880 - A Maddening Migration of an Esophageal Stent, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Alabama at Birmingham Heersink School of Medicine, Homewood, AL; 2University of Alabama at Birmingham, Birmingham, AL; 3University of Alabama at Birmingham Heersink School of Medicine, Birmingham, AL; 4Basil I. Hirschowitz Endoscopic Center of Excellence, The University of Alabama at Birmingham Heersink School of Medicine, Birmingham, AL
Introduction: Fully covered stents are a tool for the endoscopist in the management of benign and malignant strictures of the esophagus. Nevertheless, they come with potential risks to the patient, such as stent migration and related complications. Retrieval of these stents can be challenging, especially if they reach the small bowel. Here, we present a case of a migrated esophageal stent to the jejunum which was successfully retrieved via double-balloon enteroscopy (DBE) with fluoroscopic guidance.
Case Description/Methods: The patient is a 48-year-old woman with a history of ulcerative esophagitis complicated by esophageal stricture. The patient originally underwent an esophagogastroduodenoscopy (EGD) in which a 1.8x10 cm fully covered, self-expandable stent was placed at the site of the esophageal stricture. One month later, before a planned follow up EGD, she reported a week-long history of upper abdominal pain and fullness. EGD demonstrated that the previously deployed stent was absent from the esophagus; further investigation of the patient's stomach, duodenum, and proximal portion of the jejunum did not show the stent, either. A computed tomography abdomen and pelvis with contrast demonstrated the migrated esophageal stent in the mid-jejunum with local inflammation. The patient then underwent a DBE with fluoroscopic guidance for stent retrieval. The esophageal stent was successfully located in the distal jejunum and the retrieval of the stent was accomplished via SpyBite forceps [Please refer to video for procedure]. Following the DBE, a small bowel follow through confirmed no perforation or evidence of gastric leak.
Discussion: This case highlights one of the most common complications associated with esophageal stent placement. Stent migration rates vary widely, with some estimates as low as 4% but other estimates ranging as high as 30%. A large portion of stent migrations are asymptomatic. In some cases, such as when the stent remains in the stomach, a conservative approach can be taken (leaving the stent in place). However, when the stent migrates further into the gastrointestinal tract (such as into the small bowel), chances for complications increase (mucosal ulceration, obstruction, perforation) and they become more difficult to retrieve. DBE provides a less invasive, non-surgical approach to retrieve these stents. This case highlights a key therapeutic technique by DBE that should strongly be considered before surgical intervention/retrieval of the stent.
Disclosures:
Charles Evers indicated no relevant financial relationships.
Thomas Ruli indicated no relevant financial relationships.
John Cooper indicated no relevant financial relationships.
Mahmoud Aryan indicated no relevant financial relationships.
Ethan Pollack indicated no relevant financial relationships.
Ramzi Mulki indicated no relevant financial relationships.
Kabir Baig Kyanum: Olympus Medical – Consultant.
Sergio Sanchez-Luna indicated no relevant financial relationships.
Ali Ahmed: Pentax Medical – Consultant.
Shajan Peter: Olympus – Consultant.
Charles D. Evers, MD, MBA1, Thomas Ruli, MD2, John A. Cooper, MD3, Mahmoud Aryan, MD3, Ethan D. Pollack, MS, MD3, Ramzi Mulki, MD4, Kabir Baig Kyanum, MD4, Sergio Sanchez-Luna, MD4, Ali Ahmed, MD4, Shajan Peter, MD4. P3880 - A Maddening Migration of an Esophageal Stent, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
