Tuesday Poster Session
Category: Endoscopy Video Forum
P3885 - Novel Method of Treating a Malignant Esophageal Perforation via Endoscopic Vacuum Assisted Wound Closure (EVAC) by Overtube
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- SG
Subhash Garikipati, MD
Virginia Tech Carilion School of Medicine
Roanoke, VA
Presenting Author(s)
Subhash Garikipati, MD1, Kathryn Voegtlin, MSc1, Reid Wasserman, DO1, Jay Bapaye, MD1, Vivek Kesar, MD2, Paul Yeaton, MD3, Varun Kesar, MD2
1Virginia Tech Carilion School of Medicine, Roanoke, VA; 2Carilion Clinic, Roanoke, VA; 3Carilion Clinic Virginia Tech, Roanoke, VA
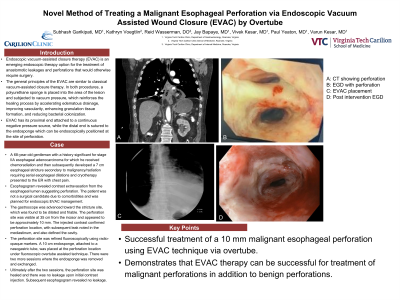
Introduction: Endoscopic vacuum-assisted closure therapy (EVAC) is an emerging endoscopic therapy option for the treatment of anastomotic leakages and perforations that would otherwise require surgery. The general principles of the EVAC are similar to classical vacuum-assisted closure therapy. In both procedures, a polyurethane sponge is placed into the area of the lesion and subjected to vacuum pressure, which reinforces the healing process by accelerating edematous drainage, improving vascularity, enhancing granulation tissue formation, and reducing bacterial colonization. EVAC has its proximal end attached to a continuous negative pressure source, while the distal end is sutured to the endosponge which can be endoscopically positioned at the site of perforation.
Case Description/Methods: A 68-year-old man with a history significant for stage IIA esophageal adenocarcinoma for which he received chemoradiation and then subsequently developed a 7 cm esophageal stricture secondary to malignancy/radiation requiring serial esophageal dilations and cryotherapy presented to the emergency room with chest pain. Esophagogram revealed contrast extravasation from the esophageal lumen suggesting perforation. The patient was not a surgical candidate due to comorbidities and was planned for endoscopic EVAC management. The gastroscope was advanced toward the stricture site, which was found to be dilated and friable. The perforation site was visible at 35 cm from the incisor and appeared to be approximately 10 mm. The injected contrast confirmed perforation location, with subsequent leak noted in the mediastinum, and also defined the cavity. The perforation site was refined fluoroscopically using radio-opaque markers. A 10 cm endosponge, attached to a nasogastric tube, was placed at the perforation location under fluoroscopic overtube assisted technique. There were 2 more sessions where the endosponge was removed and exchanged. Ultimately after the 2 sessions, the perforation site was healed and there was no leakage upon initial contrast injection. Subsequent esophagogram revealed no leakage.
Discussion: The patient was successfully treated for a 10 mm malignant esophageal perforation using a 10 cm endosponge and EVAC technique via overtube. This case demonstrates that EVAC therapy can be successful for treatment of malignant perforations in addition to benign perforations.
Disclosures:
Subhash Garikipati, MD1, Kathryn Voegtlin, MSc1, Reid Wasserman, DO1, Jay Bapaye, MD1, Vivek Kesar, MD2, Paul Yeaton, MD3, Varun Kesar, MD2. P3885 - Novel Method of Treating a Malignant Esophageal Perforation via Endoscopic Vacuum Assisted Wound Closure (EVAC) by Overtube, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Virginia Tech Carilion School of Medicine, Roanoke, VA; 2Carilion Clinic, Roanoke, VA; 3Carilion Clinic Virginia Tech, Roanoke, VA
Introduction: Endoscopic vacuum-assisted closure therapy (EVAC) is an emerging endoscopic therapy option for the treatment of anastomotic leakages and perforations that would otherwise require surgery. The general principles of the EVAC are similar to classical vacuum-assisted closure therapy. In both procedures, a polyurethane sponge is placed into the area of the lesion and subjected to vacuum pressure, which reinforces the healing process by accelerating edematous drainage, improving vascularity, enhancing granulation tissue formation, and reducing bacterial colonization. EVAC has its proximal end attached to a continuous negative pressure source, while the distal end is sutured to the endosponge which can be endoscopically positioned at the site of perforation.
Case Description/Methods: A 68-year-old man with a history significant for stage IIA esophageal adenocarcinoma for which he received chemoradiation and then subsequently developed a 7 cm esophageal stricture secondary to malignancy/radiation requiring serial esophageal dilations and cryotherapy presented to the emergency room with chest pain. Esophagogram revealed contrast extravasation from the esophageal lumen suggesting perforation. The patient was not a surgical candidate due to comorbidities and was planned for endoscopic EVAC management. The gastroscope was advanced toward the stricture site, which was found to be dilated and friable. The perforation site was visible at 35 cm from the incisor and appeared to be approximately 10 mm. The injected contrast confirmed perforation location, with subsequent leak noted in the mediastinum, and also defined the cavity. The perforation site was refined fluoroscopically using radio-opaque markers. A 10 cm endosponge, attached to a nasogastric tube, was placed at the perforation location under fluoroscopic overtube assisted technique. There were 2 more sessions where the endosponge was removed and exchanged. Ultimately after the 2 sessions, the perforation site was healed and there was no leakage upon initial contrast injection. Subsequent esophagogram revealed no leakage.
Discussion: The patient was successfully treated for a 10 mm malignant esophageal perforation using a 10 cm endosponge and EVAC technique via overtube. This case demonstrates that EVAC therapy can be successful for treatment of malignant perforations in addition to benign perforations.
Disclosures:
Subhash Garikipati indicated no relevant financial relationships.
Kathryn Voegtlin indicated no relevant financial relationships.
Reid Wasserman indicated no relevant financial relationships.
Jay Bapaye indicated no relevant financial relationships.
Vivek Kesar indicated no relevant financial relationships.
Paul Yeaton indicated no relevant financial relationships.
Varun Kesar indicated no relevant financial relationships.
Subhash Garikipati, MD1, Kathryn Voegtlin, MSc1, Reid Wasserman, DO1, Jay Bapaye, MD1, Vivek Kesar, MD2, Paul Yeaton, MD3, Varun Kesar, MD2. P3885 - Novel Method of Treating a Malignant Esophageal Perforation via Endoscopic Vacuum Assisted Wound Closure (EVAC) by Overtube, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
